Healthcare providers often face Denial Code 50, a common but challenging issue in medical billing. Imagine delivering essential care, only to have the insurer deem it “not medically necessary.” This isn’t just a clerical mistake; it disrupts cash flow and strains patient relationships.
In 2024, 38% of healthcare providers reported having at least one claim denied, with some seeing denial rates over 15%. Medical necessity denials account for $2.5 billion in annual losses.
Understanding Denial Code CO 50 is critical for billing teams. A proactive approach can save time, resources, and ensure patients get the care they need without unnecessary financial setbacks.
What Is Denial Code 50?
Denial Code CO 50 typically means that the service billed does not meet the insurer’s medical necessity criteria and is therefore deemed non-covered. This denial code can occur for several reasons, but it’s most often seen when the insurer believes that the procedure or treatment isn’t necessary according to their policies.
Denial Code 50 typically refers to:
“These services are not covered as they are not considered a ‘medical necessity’ by the payer.”
In the context of Medicare, Denial Code CO 50 is paired with Remark Code N115, which indicates that the denial is based on Local Coverage Determination (LCD) or National Coverage Determination (NCD) policies. This type of denial is considered a contractual obligation and cannot be corrected or resubmitted automatically. Providers must submit a formal redetermination or appeal within the payer’s filing deadline. For effective denials management, it’s crucial for providers to track these types of denials closely and implement strategies to address them proactively.
Example:
A cardiologist orders a stress echocardiogram for a patient with chest pain. The insurer rejects the claim with CO 50, indicating that the service isn’t medically necessary. Why?
The diagnosis code used was R07.89 (Other chest pain), which did not meet Medicare’s criteria. Instead, a more specific code, such as I20.0 (Unstable angina), would have been required for the procedure to be covered.
Reason Code 50 & Remark Code N115
In medical billing, when a claim is denied with Reason Code 50 and Remark Code N115, it means the payer believes the service provided was not medically necessary under their coverage policy.
| Code | Description |
| Reason Code 50 | Non-covered services are because that are not deemed medically necessary by the payer. |
| Remark Code N115 | The decision is based on a Local Coverage Determination (LCD) or National Coverage Determination (NCD). |
Payer-Specific Differences in CO 50 Denials
Denial Code CO 50 may appear across all payers, but the criteria for what’s deemed “medically necessary” can vary.
- Medicare relies on LCDs/NCDs, and denials often include Remark Code N115. These guidelines are publicly available and specific.
- Medicaid rules differ by state, and services considered medically necessary in one state may not be in another. Always refer to your state’s Medicaid manual.
- Commercial payers like UHC or BCBS follow their internal policies and may apply CO 50 for services deemed experimental, cosmetic, or lacking documentation. They may also have stricter frequency limits or require prior authorization.
- Other Commercial Insurance some payers apply CO 50 for services not considered part of their covered benefits, such as investigational or elective services. These services might be denied because they fall outside the terms of the patient’s policy, and resolving these denials requires contacting the payer for more information
Common Causes of Denial Code 50
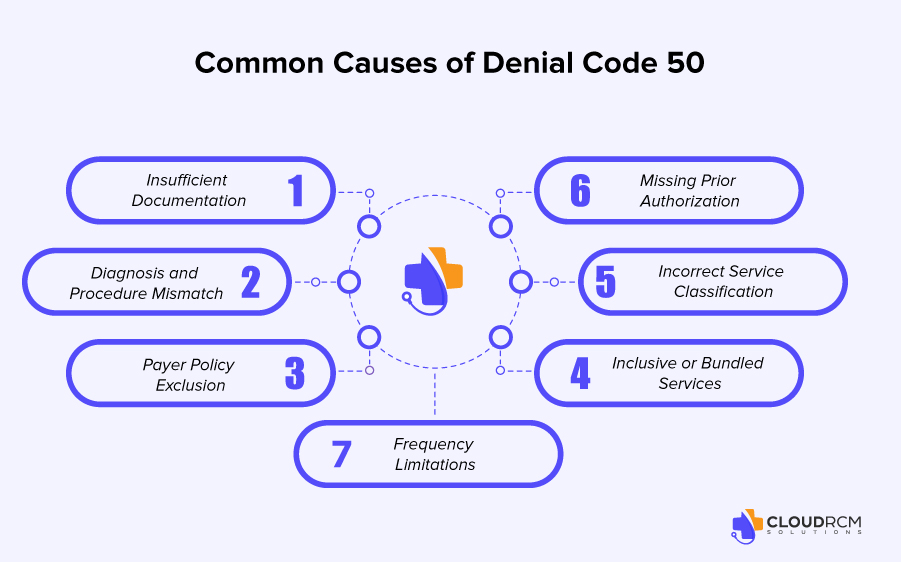
CO-50 denial code is a common denial in medical billing and can result in payment delays or revenue loss if not addressed promptly. Below are the typical reasons behind this denial
- Insufficient Documentation:
If the clinical notes don’t clearly explain why a service was medically necessary, it’s likely to be denied. Proper documentation that justifies the diagnosis and the treatment plan is essential for proving the medical necessity of a service. - Diagnosis and Procedure Mismatch:
If the diagnosis code doesn’t match the billed procedure, the insurer may not deem the service necessary. For example, a diagnosis code indicating a mild condition may not be sufficient to justify the need for a major surgical procedure. - Payer Policy Exclusions:
Some services may fall under exclusions in the payer’s policy, such as experimental treatments, cosmetic procedures, or services rendered outside the coverage guidelines. It’s critical to verify coverage before providing certain types of care, especially when dealing with high-cost or elective treatments. - Frequency Limitations:
Payers impose restrictions on the frequency with which certain services can be rendered. For instance, if a service is repeated more than the allowable limit, it could be denied. Healthcare providers must track how often certain services are provided to avoid exceeding these limits. - Incorrect Service Classification:
Services may be incorrectly classified as preventive when they should be diagnostic, or vice versa. Without proper classification, the payer may refuse coverage. Providers must classify services correctly based on their intent and documentation. - Missing Prior Authorization:
For services that require prior authorization, failure to obtain this pre-approval will likely result in a CO 50 denial. It’s important to check each payer’s guidelines to determine if pre-authorization is necessary before providing the service. - Inclusive or Bundled Services:
Sometimes, the billed service is considered part of another, larger procedure and isn’t reimbursed separately. For example, certain surgical procedures may include anesthesia, and billing both separately could lead to a denial.
5 Steps to Appeal a Denial Code CO 50
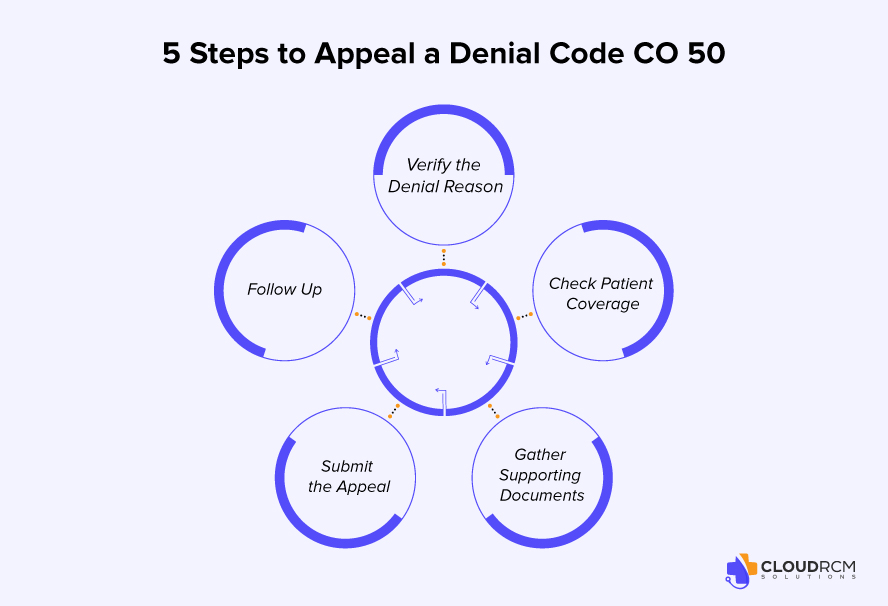
A CO 50 denial means the service is considered “not covered” by the payer, but in many cases, an appeal can reverse the decision. Here’s a simplified guide to help billing staff take the right steps:
1. Verify the Denial Reason
Check the Explanation of Benefits (EOB) or ERA to confirm the reason for denial. It could be due to incorrect coding, missing information, or a misunderstanding of coverage.
2. Check Patient Coverage
Ensure the patient had active coverage on the service date. Review the payer’s coverage policies or LCD/NCD guidelines to see if the service should be covered under certain conditions.
3. Gather Supporting Documents
Collect physician notes, test results, referrals, and any other records that support the medical necessity of the denied service.
4. Submit the Appeal
Write a brief appeal letter explaining why the service should be covered. Include patient and claim details, a summary of the issue, and attach all supporting documents.
5. Follow Up
Track the appeal status through the payer portal or by contacting the payer directly. Be ready to provide more information or escalate the appeal if needed.
How to Avoid This Denial
Ensure complete and clear documentation, verify payer coverage policies, use accurate codes, and confirm any prior authorization requirements. Staying proactive with billing protocols significantly reduces the chance of Denial Code 50.
Tips to Prevent CO 50
There are several ways you can prevent the denial code CO 50:
Verify Medical Necessity Guidelines
Review the payer’s medical necessity policies and ensure the service is covered for the patient’s diagnosis before rendering care.
Use Accurate and Specific Diagnosis Codes
Assign diagnosis codes that support the medical need for the procedure or service provided.
Submit Complete Clinical Documentation
Include detailed progress notes, test results, and treatment plans that justify why the service was required.
Check Prior Authorization Requirements
Confirm whether the procedure needs pre-approval and obtain it before delivering the service.
Avoid Frequency Limit Violations
Track how often certain services have been provided to avoid exceeding payer-defined limits.
Understand Payer-Specific Coverage Policies
Be aware of exclusions like cosmetic or investigational services that the plan may not cover.
Code Services Correctly (Preventive vs. Diagnostic)
Ensure that services are properly classified to reflect their intent, especially when coding preventive or diagnostic care.
Use Medical Necessity Tools
Utilize payer tools (like Medicare LCD/NCD policies) or third-party software to check medical necessity alignment before billing.
Final thought:
Denial Code CO 50 can be frustrating, but it doesn’t have to disrupt your revenue cycle. By understanding payer-specific medical necessity rules, improving documentation practices, and proactively verifying coverage, providers can minimize denials and strengthen their appeal success rate. The key is to treat each CO 50 denial not as a dead end, but as an opportunity to refine your billing workflow and ensure patients receive the care they need without reimbursement barriers. Stay informed, stay compliant, and stay proactive.
How CloudRCM Helps with CO 50 Denials
CloudRCM is here to help healthcare providers navigate the complexities of CO 50 denials and medical necessity issues. Our experts identify gaps in coding and documentation before submission, helping to prevent denials from the start. If claims are denied, we act quickly with strong appeals, referencing payer-specific guidelines to increase the likelihood of success.
Need help resolving Denial Code 50? Schedule an appointment with our billing experts today and get the support you need to navigate and prevent these denials.
FAQ’s
How to handle CO 50 denial?
Review the payer’s medical necessity criteria, correct any documentation or coding issues, and submit a well-supported appeal with all required records.
What is claim adjustment reason code 50?
Code 50 means the service is not covered because the payer deems it not medically necessary under their policy.
What is occurrence code 50 used for?
Occurrence code 50 indicates the start date of hospice care for billing hospice-related services.
What is a remark code for medical necessity?
Common remark codes like N115 explain that the denial is based on a Local or National Coverage Determination (LCD/NCD) regarding medical necessity.
What is a CO 50 remark code?
A CO 50 denial often pairs with Remark Code N115, meaning the service was denied due to payer policies defining it as not medically necessary.
What should you do if a claim is denied due to medical necessity?
Review the denial, ensure proper documentation and diagnosis coding, and submit an appeal with evidence supporting the medical need for the service.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine