Telehealth isn’t the problem in 2026 getting paid is. With nearly 30% of patient visits now virtual, telehealth has become a permanent part of healthcare delivery. Despite rising demand, many practices are seeing telehealth revenue slip through the cracks.
The issue isn’t documentation or patient volume. It’s credentialing gaps, billing errors, and constantly changing payer rules. These breakdowns are driving higher telehealth claim denials, delayed reimbursements, and avoidable revenue loss. Practices that don’t tighten their telehealth billing workflows in 2026 risk turning virtual care into a financial liability instead of a growth engine.
Telehealth Claim Denials: Understanding the Core Issues
As the role of telehealth expands, so do the challenges associated with telehealth billing. In 2026, telehealth claim denials are emerging as a significant roadblock to revenue generation for many healthcare providers. The key reasons contributing to claim denials include credentialing gaps, billing inaccuracies, and payer policy variability. Understanding each of these barriers is essential for practices to reduce AR days and avoid lost revenue.
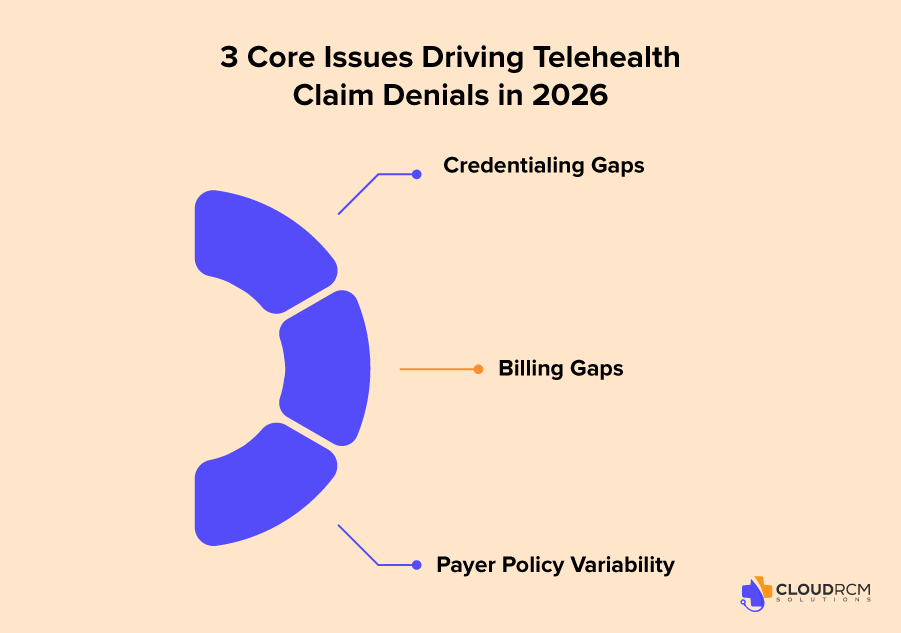
1. Credentialing Gaps: A Primary Driver of Telehealth Denials
Credentialing is a critical step for providers offering telehealth services, but it is often overlooked. Many practices continue to face credentialing issues, where providers are not properly enrolled for telehealth services, even though they are credentialed for in-person visits. This problem is especially prevalent in states with high Medicare and Medicaid populations, such as California, Texas, and New York.
A report from the American Medical Association (AMA) shows that nearly 25% of telehealth claims are delayed or denied due to missing or incomplete credentialing documentation. Practices in rural or underserved areas face even more difficulty, as telehealth services are crucial to reaching patients but remain hindered by credentialing bottlenecks.
Example:
A New York-based internal medicine practice was recently forced to write off over $15,000 in telehealth claims after discovering that one of their providers wasn’t credentialed to offer telehealth services for Medicare Advantage patients. The claims were correctly coded and documented, but the lack of proper payer enrollment led to automatic denials.
Practices should ensure that all telehealth providers are properly enrolled with all relevant payers, especially Medicare, Medicaid, and private insurers, and should review credentialing records regularly.
2. Billing Gaps: How They Contribute to Denials
Billing for telehealth services requires specific billing codes and modifiers that differ from traditional in-person visits. Misapplication of CPT codes, the failure to include modifiers (such as GT or 95), and incorrect place-of-service codes are common reasons for telehealth claim rejections.
- Incorrect CPT Codes: Many practices still use CPT codes for in-person visits, leading to denied claims when the correct telehealth-specific codes aren’t used.
- Modifiers for Telehealth: Telehealth visits require specific modifiers, and without these, claims will be rejected.
- Patient Location and Eligibility: Insurers may require patients to be located in certain regions (e.g., rural areas) for telehealth coverage, but this information is often omitted, leading to denials.
Example:
A Texas pediatric practice submitted a claim for a telehealth consultation but failed to use the appropriate POS 02 code, causing the insurer to reject the claim. In this case, the error was simply a misunderstanding of the billing requirements, leading to delays in payment.
Practices should standardize telehealth billing processes, ensuring all appropriate CPT codes, modifiers, and place-of-service codes are used correctly.
3. Payer Policy Variability: The Impact on Telehealth Claims
Another major issue contributing to telehealth claim denials is the inconsistency in payer rules. Different payers including Medicare, Medicaid, and private insurers have different requirements when it comes to telehealth services. This variability creates confusion among providers and billing teams, resulting in claim denials.
- Medicare: While Medicare covers telehealth services, coverage often depends on the patient’s location and the type of telehealth service being provided.
- Medicaid: Medicaid rules for telehealth vary significantly by state, with some states reimbursing telehealth services more generously than others.
- Commercial Insurers: Some commercial insurers reimburse for specific types of care, while others refuse reimbursement altogether.
Example:
A California-based family medicine clinic faced denial of over 30 telehealth claims due to a misunderstanding of Medicare Advantage rules. The claims were rejected because the clinic had failed to submit the right modifiers required by the payer, even though the services were clearly telehealth consultations.
Practices should stay up-to-date with payer rules and ensure that they are in compliance with the latest telehealth regulations. Investing in automated billing systems can help reduce errors.
Telehealth Claim Denials Across Specialties: Challenges and Key Statistics
| Specialty | Telehealth Use | Credentialing & Billing Challenges | States Affected | Claim Denial Rate | Key Statistics |
| Internal Medicine | Routine visits, chronic disease management, follow-up care | Credentialing issues with private insurers; delayed claims due to payer-specific requirements not updated for telehealth | California, New York | 25% | 25% of claims delayed/denied due to credentialing issues (MGMA Study) |
| Behavioral Health | Virtual consultations, especially for mental health services | Improper credentialing and unclear billing practices; increased scrutiny from Medicaid | Florida, Texas | 40% | 40% of telehealth claims denied due to credentialing and billing errors (American Psychological Association, 2025) |
| Pediatrics | Follow-ups and minor illnesses | Discrepancies in billing codes for telehealth services; separate telehealth policies for commercial insurers | Illinois, Ohio | High | Pediatric claims commonly denied due to code discrepancies between telehealth and in-person services |
| Family Medicine | General patient consultations, routine check-ups | Payer restrictions on telehealth service types; unclear payer rule communication | Nationwide | 20% | 20% of family medicine telehealth claims denied due to unclear payer rules (AAFP, 2025) |
| Specialty Care | Dermatology, neurology, cardiology telehealth consultations | Variations in credentialing requirements between insurers; lack of proper documentation for visual exams in dermatology | Georgia, Arizona | Higher than average | Dermatology telehealth claims often denied due to lack of insurer-specific telehealth standards and documentation issues |
How to Minimize Telehealth Claim Denials in 2026
Now that we’ve explored the primary reasons behind telehealth claim denials, let’s discuss actionable best practices to minimize these denials and improve revenue collection in 2026.
1. Standardize Telehealth Billing Processes
Ensure that your practice has a standardized workflow for telehealth billing that includes correct CPT codes, place-of-service codes, and modifiers (e.g., GT, 95). This will reduce billing errors and denial rates.
2. Update Credentialing Records Regularly
- Make sure all telehealth providers are properly credentialed with all Medicare, Medicaid, and private insurance payers.
- Review credentialing records annually to ensure that your telehealth providers are properly enrolled with all relevant payers.
3. Proactively Track Authorizations
Monitor authorization dates and submit renewals before they expire. This proactive approach helps prevent claims from being denied due to missing or expired prior authorization.
4. Use AI-Powered Billing Solutions
- Implement automated billing systems that are designed to help with denial management and claims tracking.
- These systems can identify common denial reasons, track payer-specific rules, and ensure compliance, minimizing revenue loss and reducing AR days.
How Cloud RCM Solutions Supports Telehealth Practices
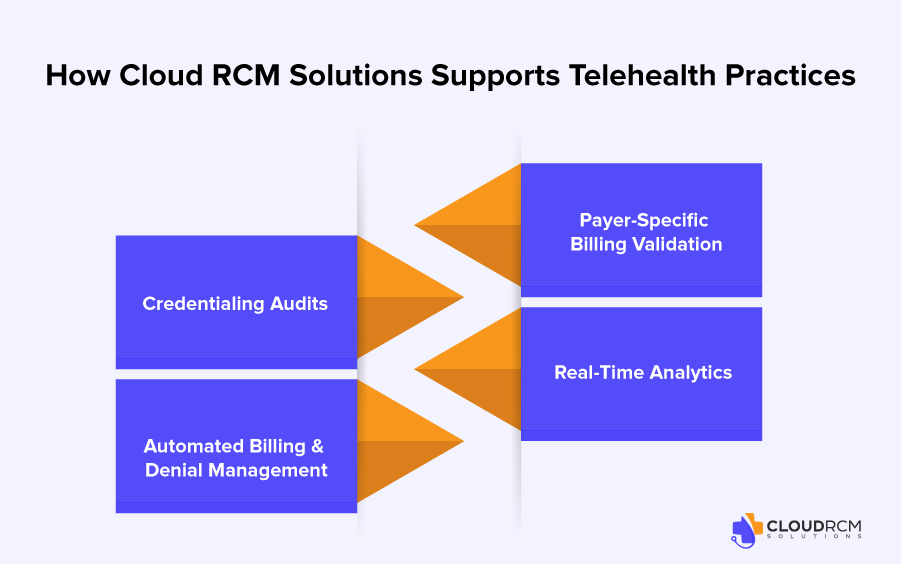
Cloud RCM Solutions specializes in addressing the challenges of telehealth billing. By focusing on credentialing, billing accuracy, and payer-specific compliance, we help telehealth providers minimize claim denials and reduce AR days.
Here’s how Cloud RCM Solutions can support your practice:
- Credentialing Audits: We proactively audit credentialing records, ensuring that all telehealth providers are properly enrolled with relevant payers.
- Automated Billing & Denial Management: Our AI-powered billing system tracks denials in real-time, automatically generating appeals and adjustments to speed up payment recovery.
- Payer-Specific Billing Validation: We ensure that your practice complies with Medicare, Medicaid, and commercial payer rules for telehealth, reducing errors and minimizing claim rejections.
- Real-Time Analytics: Our advanced analytics provide visibility into your telehealth AR, allowing your practice to track payer performance, monitor AR aging, and optimize your revenue cycle.
By partnering with Cloud RCM Solutions, your telehealth practice can reduce claim denials, shorten AR days, and maximize revenue collection.
Conclusion:
In 2026, telehealth remains a key pillar of healthcare delivery, but credentialing gaps, billing inaccuracies, and payer rule inconsistencies continue to hinder revenue. To maximize telehealth revenue, healthcare practices must streamline their billing processes, stay compliant with payer rules, and ensure that credentialing is properly handled.
With Cloud RCM Solutions, you can reduce claim denials, optimize your telehealth billing workflow, and ensure faster reimbursements. By addressing credentialing, billing, and payer rule issues upfront, your practice can unlock the full potential of telehealth in 2026.Learn how Cloud RCM Solutions can help streamline your telehealth revenue cycle and minimize claim denials today. Contact us for a personalized consultation!
FAQ’s
Why is telehealth credentialing more difficult in 2026?
Telehealth credentialing is more complex due to multi-state licensure requirements, payer-specific telehealth rules, and frequent Medicare policy updates that affect enrollment and reimbursement.
What causes telehealth claims to be denied most often?
Common denial reasons include incorrect place-of-service codes, missing telehealth modifiers, inactive payer enrollment, and services billed in states where providers are not credentialed.
How do enrollment errors impact telehealth reimbursement?
Enrollment errors can lead to claim denials, delayed payments, and post-payment audits, even when services are clinically appropriate and properly documented.
Does Medicare require special credentialing for telehealth services?
Yes. Medicare telehealth services must meet specific credentialing, enrollment, and billing requirements that differ from in-person care and continue to change in 2026.
Why is multi-state payer enrollment important for telehealth practices?
Telehealth providers must be enrolled with payers in each state where patients are located. Without multi-state enrollment, claims are often denied regardless of medical necessity.
How does credentialing affect telehealth claim approval time?
Incomplete or outdated credentialing increases claim review time, manual audits, and payer follow-ups, leading to longer accounts receivable cycles.
What happens if telehealth recredentialing is missed?
Missed recredentialing can result in sudden claim denials, payment holds, or payer termination, causing unexpected revenue disruptions.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine