Are billing errors, denials, and delayed payments draining your anesthesia practice? You’re not alone. As we step into 2026, anesthesia billing is more complicated than ever. From the evolving regulatory landscape to the complexities of time-based billing, anesthesia providers are facing new challenges at every turn. Payer policies are shifting, documentation requirements are becoming stricter, and the need for precise coding has never been more critical. For solo practices, mid-sized groups, and large hospitals alike, staying on top of anesthesia billing is now essential. It’s key to securing accurate reimbursements and maintaining your practice’s financial health
If you’re tired of the constant denial letters, payment delays, and confusion over codes, it’s time to rethink your strategy. 2026 demands that providers adapt and streamline their billing processes to thrive in a fast-evolving healthcare environment.
The Significance of Anesthesia Billing for Hospitals in 2026
Anesthesia billing plays a critical role in the financial health of hospitals and providers. With the constant advancements in anesthetic procedures and the evolving health profiles of patients, accurate billing has become more essential than ever. In fact, between 2021 and 2023, anesthesia billing rates saw a 3% increase, reflecting the need for higher ASA classifications due to an aging population and changing healthcare regulations.
Why is this important? Anesthesia billing not only impacts a hospital’s ability to generate revenue but also determines how well it can adhere to regulatory guidelines. As the healthcare industry evolves, so must the billing practices. Hospitals must adopt modern billing strategies to stay financially stable and compliant.
How ASA Classification Impacts Anesthesia Billing in 2026
The American Society of Anesthesiologists (ASA) classification system remains a core component of anesthesia billing. It helps determine the complexity and risk of anesthesia services based on the patient’s health. With more complex cases due to an aging population, correctly applying ASA classifications is crucial for accurate billing and appropriate reimbursement.
Here’s a breakdown of how ASA classifications affect anesthesia billing:
| ASA Classification | Description | Example |
| ASA I | Healthy, low-risk patient | A young, healthy patient undergoing a minor procedure |
| ASA II | Mild systemic disease | A patient with controlled hypertension or mild obesity |
| ASA III | Severe disease, not life-threatening | A patient with chronic heart disease or poorly controlled diabetes |
| ASA IV | Life-threatening condition | A patient with unstable angina or severe kidney disease |
| ASA V | Moribund patient needing surgery | A patient with severe trauma or ruptured aneurysm |
| ASA VI | Brain-dead patient for organ donation | A brain-dead patient whose organs are being harvested |
| ASA (E) | Emergency procedure | A patient requiring surgery to avoid significant life-threatening risks |
The ASA classification system helps providers assess the risk level, ensuring that anesthesia services are billed appropriately.
Anesthesia Billing Process for Hospitals
Billing for anesthesia services in hospitals isn’t just about coding procedures; it’s a multi-step process involving base units, time units, and modifier units. Here’s how it works:
1. Base Units
Base units reflect the complexity of the anesthesia procedure. The CPT code used determines the base unit value, which is crucial for validating payment and ensuring correct reimbursement.
2. Time Units
Time is a major factor in anesthesia billing. Medicare and other payers often pay based on time units, calculated in 15-minute intervals. The contract terms differ by payer, with some specifying 4 units per hour and others 5 units. Accurate tracking of anesthesia time is essential to ensure the correct payment.
3. Modifier Units
Modifier units adjust billing based on patient conditions, such as age, physical health, or the need for supervision by a CRNA. Factors like controlled hypotension, emergency cases, and unusual positions can all impact the modifier units. Using the correct modifiers is essential to avoid underpayment or denied claims.
4. The Anesthesia Billing Formula
The billing formula is simple but crucial:
(Base Units + Time Units + Modifier Units) × Conversion Factor = Anesthesia Fee
The conversion factor changes annually and varies by location, reflecting regional differences in healthcare costs.
Core Components of Anesthesia Services
Anesthesia services are generally divided into three parts, all of which factor into billing:
- Pre-Anesthesia Evaluation:
This is a thorough assessment of the patient’s health before anesthesia is administered. It includes gathering key information about the patient’s medical history and current health condition.
- Anesthesia Time:
This is the actual time spent administering anesthesia to the patient. Accurate tracking of the time ensures proper reimbursement.
- Post-Anesthesia Care:
After the procedure, the patient is monitored until they have sufficiently recovered from the anesthesia. This post-care period is also factored into the overall billing.
These three components form the “anesthesia package” for hospitals, and it’s essential that they are documented and billed properly to ensure full reimbursement.
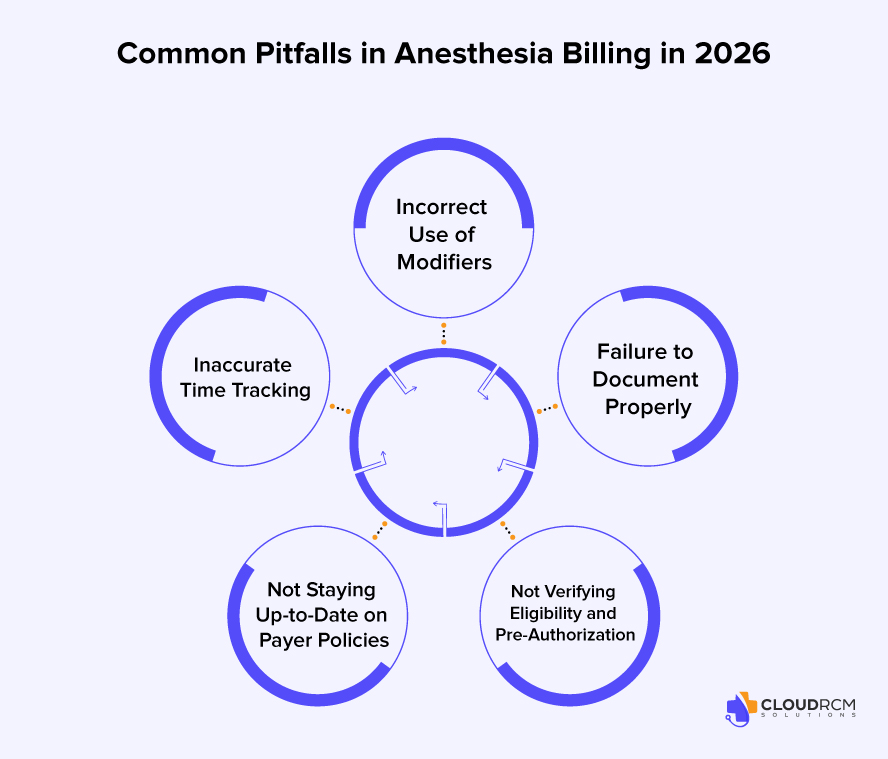
Why Anesthesia Billing is More Complex Than Ever in 2026
Anesthesia billing in 2026 presents several challenges that make it more complex and demanding than before. The following factors contribute to the increasing difficulty for providers:
- Time-Based Billing: Accuracy is Crucial
Anesthesia billing relies heavily on tracking time in 15-minute increments. Given the nature of anesthesia services, any error in tracking time whether through manual calculation or misreporting can lead to underbilling or potential audit risks. Ensuring every minute is accurately recorded is essential for preventing lost revenue and complying with payer expectations.
- Complicated ASA Classifications
The American Society of Anesthesiologists (ASA) Classification plays a vital role in determining the complexity and pricing of anesthesia services. As patient conditions become more complex due to aging populations and chronic illnesses, accurately assigning the right ASA level is increasingly challenging. Misclassification can lead to undercharging for high-risk patients or overestimating risk for lower-risk ones.
- Diverse Payer Rules and Modifier Use
Different payers Medicare, Medicaid, and private insurers have varying rules, making billing for anesthesia services a moving target. Providers must apply the correct modifiers such as QK, QZ, and AA to adjust payment rates based on the level of service provided. Using the wrong modifier can lead to claim rejections, affecting timely reimbursements.
- Documentation Must Be Flawless
In anesthesia billing, documentation is just as important as coding. Anesthesia services require detailed and accurate documentation, including medication administered, start and stop times, and the patient’s physical condition. Small errors in documentation can result in denied claims and can even trigger audits, delaying payments and disrupting cash flow.
- High Denial Rates and Lengthy Appeals
Anesthesia billing is susceptible to a higher denial rate due to issues like incorrect codes, missing modifiers, and inaccurate patient information. Denied claims require time-consuming appeals, which contribute to slower cash flow and add more administrative work. Managing these denials effectively is crucial to maintaining the financial health of the practice.
How to Overcome Anesthesia Billing Challenges in 2026
To navigate the increasingly complex landscape of anesthesia billing in 2026, providers must adopt strategies and tools that not only simplify processes but also improve accuracy and reduce administrative burdens. Here’s how to tackle these challenges head-on:
1. Leverage Automated Time Tracking Tools
Accurate time tracking is the foundation of anesthesia billing. Adopting automated time tracking systems can help eliminate the risk of manual errors. These tools capture start and stop times in real-time, reducing the chances of underbilling or misreporting. With automation, you can ensure that every minute of anesthesia is correctly recorded and billed, improving both efficiency and reimbursement accuracy.
2. Stay Updated on ASA Classifications
As ASA classifications continue to evolve, it’s essential for anesthesia providers to stay informed about the latest updates in patient health trends and classification guidelines. Regular training for your team and integration of electronic health record (EHR) systems that automatically apply ASA classifications based on documented patient information can streamline the process. This reduces errors and ensures that you’re charging appropriately based on the complexity of the procedure.
3. Use Advanced Coding Software and Modifier Checkers
Incorporating coding software that automatically checks for correct CPT codes and modifiers can significantly reduce the chances of errors. These systems allow for real-time coding adjustments based on the procedure, patient status, and payer-specific rules, helping to prevent denials due to incorrect modifiers or missing information. Additionally, by integrating modifier-checking tools, you ensure your billing process aligns with payer expectations.
4. Improve Documentation with Digital Solutions
Documentation is often the source of many billing issues. Implementing digital documentation tools and EHR systems can help you capture all necessary details, including medication administered, patient status, and procedure specifics. This ensures compliance with Medicare, Medicaid, and other insurance providers, helping you avoid denials due to incomplete or incorrect records. Having these records digitally stored and easily accessible also speeds up the billing process, reducing delays in payment.
5. Focus on Denial Prevention with a Proactive Strategy
The best way to handle denials is to prevent them in the first place. Develop a denial management strategy that focuses on identifying potential issues before claims are submitted. Use real-time claim tracking systems to catch common errors such as missing modifiers or incorrect codes, early in the process. Also, implementing a dedicated denial management team or outsourcing this task can help address issues quickly and reduce the time spent on appeals, ultimately improving cash flow.
6. Outsource to Anesthesia Billing Experts
For many providers, outsourcing anesthesia billing to specialized billing companies can save time, reduce errors, and improve reimbursement rates. These companies bring in-depth knowledge of anesthesia billing practices and are equipped to handle the complexities of the coding process, payer policies, and documentation requirements. By outsourcing, you can focus on providing quality care while leaving the billing process to experts who understand the nuances of anesthesia reimbursement.
How Anesthesia Providers Can Stay Ahead in 2026
As we move further into 2026, staying ahead in the competitive landscape of anesthesia billing requires embracing innovative technologies, continuous education, and data-driven decision-making. Here’s how anesthesia providers can adapt:
- Embrace Artificial Intelligence and Automation
Artificial intelligence is increasingly being integrated into the billing process. AI-powered billing tools can automate coding, modifier usage, and denial detection, helping you reduce human error and improve efficiency.
- Focus on Predictive Analytics
Predictive analytics tools allow practices to forecast payer behavior and predict denials before they occur. This proactive approach helps you address potential issues early, speeding up the billing process and improving cash flow.
- Invest in Continuous Training and Certification
Staying updated on the latest coding updates and regulations is crucial. Invest in ongoing education for your team to ensure they understand the newest ASA classifications, payer rules, and regulatory changes.
- Adopt a Comprehensive Compliance Strategy
In 2026, compliance with payer regulations and healthcare laws will be more complex than ever. Ensure that your practice is HIPAA-compliant, maintains auditable records, and follows payer-specific rules to avoid costly fines.
The Future of Anesthesia Billing: Trends to Watch in 2026 and Beyond
As we move toward 2026, several key trends are shaping the future of anesthesia billing. These advancements will streamline the process, improve efficiency, and ensure that providers are prepared for the evolving healthcare landscape:
| Trend | Description | Impact on Anesthesia Billing |
| AI-Powered Automation | Artificial Intelligence tools will automate coding and modifier assignments, analyzing patient and procedure data in real-time. | Reduces human error, improves accuracy, and speeds up billing. |
| Blockchain for Transparency | Blockchain technology will create secure, transparent billing records, ensuring that all information is tamper-proof and easily auditable. | Minimizes fraud and simplifies the audit trail. |
| Real-Time Data and Analytics | Predictive analytics will allow providers to forecast payer behavior and identify potential issues early. | Improves cash flow by catching issues before they affect payments. |
| Patient-Centered Billing | With more patient responsibility for costs, transparent billing will provide clear, upfront pricing for anesthesia services. | Enhances patient satisfaction and reduces billing disputes. |
| Telehealth and Virtual Services | The rise of telehealth will lead to more virtual anesthesia services, including consultations and post-care. | Providers will need to adjust billing for remote services. |
Practical Steps to Prepare for Anesthesia Billing in 2026
As anesthesia billing becomes more complex, it’s crucial to stay ahead of the curve. Here are the essential steps to ensure your practice is ready for 2026:
- Upgrade Billing Technology
Invest in AI-powered coding software and real-time tracking to improve accuracy and efficiency. - Ongoing Team Training
Regularly update your team on ASA classifications, payer policies, and new billing software to stay current. - Enhance Denial Management
Implement a proactive denial management system to catch issues early and reduce appeal time. - Switch to Digital Documentation
Adopt EHR integration to streamline documentation and ensure compliance. - Stay Updated on Regulations
Monitor changes in Medicare, Medicaid, and private payer regulations to avoid penalties and revenue loss.
How Cloud RCM Solutions Improves Anesthesia Billing in 2026
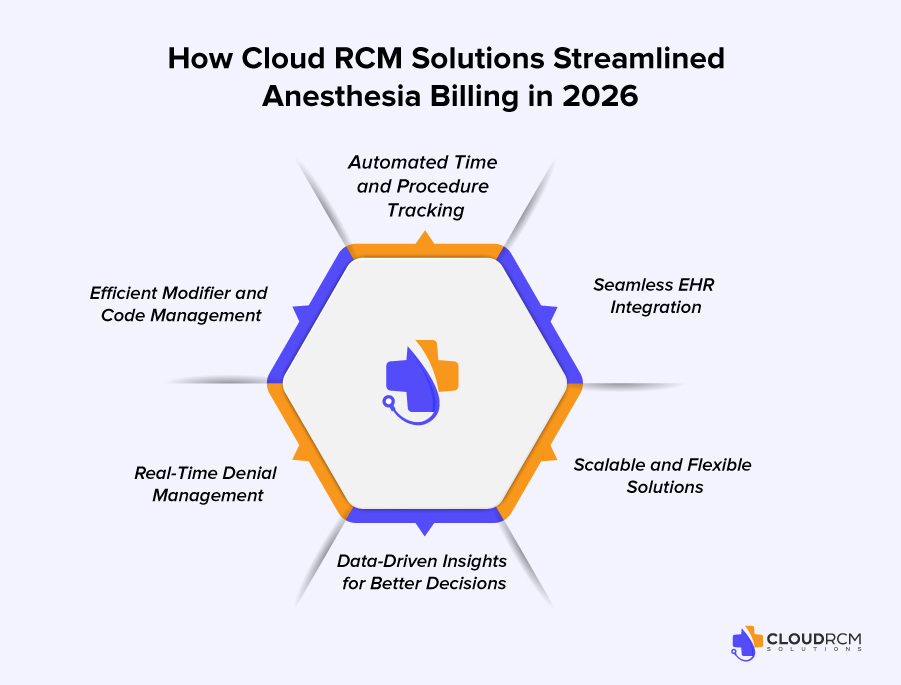
In 2026, Cloud RCM Solutions is your ticket to faster reimbursements and fewer denials. Automating time tracking and procedure recording ensures accurate billing, eliminating the risk of underbilling.
With seamless EHR integration, these solutions streamline documentation, reducing errors and denials. Automatic coding ensures claims are correctly filed the first time, boosting approval rates and speeding up payments.
Real-time denial management keeps your cash flow steady, while data-driven insights help optimize your billing strategy. Cloud RCM is scalable, ensuring your practice stays ahead whether you’re a solo provider or part of a large system.
Conclusion:
Don’t let billing errors and delays hold your practice back. Cloud RCM Solutions can streamline your anesthesia billing, reduce denials, and boost revenue. Take control of your financial health and stay ahead in 2026.
Take control of your anesthesia billing today! Contact us now and discover how Cloud RCM Solutions can maximize your revenue and eliminate billing challenges in 2026.
How do I bill for anesthesia services correctly?
Billing for anesthesia involves combining base units, time units, and modifier units, then multiplying by the conversion factor. Accurate coding, proper ASA classification, and detailed documentation are essential to ensure correct reimbursement. Errors in any of these areas can lead to claim denials or delayed payments.
What is ASA classification and why does it matter for billing?
ASA (American Society of Anesthesiologists) classification assigns a risk level to patients based on their health. The classification impacts anesthesia billing because higher-risk patients often require more complex care, which justifies higher base units and appropriate reimbursement. Misclassifying ASA levels can lead to underbilling or claim denials.
How do anesthesia time units work for reimbursement?
Anesthesia billing is time-based, typically calculated in 15-minute increments. Accurate start and stop times are critical, as payers rely on these to determine total time units. Automated time-tracking tools can reduce errors and ensure precise billing for every procedure.
What are the common reasons anesthesia claims get denied?
Claims are often denied due to incorrect ASA classification, missing or incorrect modifiers (e.g., QK, QZ, AA), inaccurate time reporting, incomplete documentation, or failure to verify patient eligibility and pre-authorization. Staying updated on payer policies is key to reducing denials.
How can I prevent claim denials in anesthesia billing?
Preventing denials requires accurate coding, thorough documentation, real-time eligibility verification, timely pre-authorization, and using proper modifiers. Leveraging automated billing tools and conducting pre-submission audits also significantly reduce claim rejections.
What modifiers do I need to use for anesthesia billing?
Common anesthesia modifiers include AA (Anesthesiologist services only), QK (Medical direction of two to four concurrent procedures), QZ (CRNA service without medical direction), and others depending on the payer. Correct modifier use ensures proper reimbursement and prevents claim denials.
Can technology or software help with anesthesia billing?
Yes. AI-powered billing tools, automated time trackers, EHR integration, and modifier checkers can reduce manual errors, improve claim accuracy, and speed up reimbursements. These tools also help with denial prevention by preemptively flagging issues
How can my practice improve reimbursement for anesthesia services?
Improving reimbursement requires accurate ASA classification, precise time tracking, proper modifier usage, complete documentation, proactive denial management, and leveraging automated billing solutions. Partnering with a specialized RCM provider can also optimize revenue and streamline workflows.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine