Behavioral health and psychiatry practices are facing significant billing challenges in 2026. With telehealth continuing as a core service, stricter payer policies, and frequent prior authorizations, Accounts Receivable (AR) days are on the rise. AR cycles extending to 60, 90, or even 120+ days are creating a financial strain, disrupting cash flow, and impeding growth for these vital practices.
Reducing AR days is no longer just a financial goal; it’s essential for the sustainability of your practice. In this blog, we’ll explore the top AR challenges in behavioral health and provide practical solutions to optimize your revenue cycle performance. We’ll also demonstrate how Cloud RCM Solution can support your practice in reducing AR days and improving financial health.
Why AR Days Are Critical in 2026:
- Extended AR slows down cash flow, affecting daily operations, payroll, and investments in technology.
- Higher AR increases administrative costs due to repeated follow-ups and claim resubmissions.
- Long AR cycles prevent practices from scaling services, hiring staff, or upgrading digital systems.
- For multi-site practices, untracked AR can create hidden bottlenecks that multiply inefficiencies across locations.
In 2025, behavioral health practices in the U.S. reported an average AR of 65–75 days, up from 50–55 days in 2024, highlighting a growing need for optimized billing workflows.
Understanding Accounts Receivable (AR) in Behavioral Health
Accounts Receivable (AR) refers to the money your practice is owed by payers, including commercial insurance, Medicare, Medicaid, and patients. The key metric for measuring AR efficiency is AR days, the number of days between the date a service is provided and when payment is received.
Why AR Matters:
- Cash Flow: Extended AR days slow down your incoming revenue, affecting daily operations, payroll, and investments in technology and growth.
- Profitability: High AR days indicate inefficiencies in your billing processes, leading to increased administrative costs and lost revenue.
- Operational Impact: The more time your staff spends chasing unpaid claims, the less time they have to focus on delivering quality care to your patients.
Understanding AR metrics allows practices to make data-driven decisions, streamline billing, and reduce revenue leakage.
Top AR Challenges in Behavioral Health / Psychiatry (2026)

Behavioral health practices face unique AR challenges that differ significantly from other medical specialties. The following factors are driving AR delays and financial inefficiencies in 2026.
1. Telehealth Billing Requirements Are Complex
Telehealth has become a cornerstone of behavioral health service delivery, particularly for therapy, psychiatry consultations, and medication management. However, telehealth billing introduces multiple complexities that frequently delay reimbursements.
One of the most common issues is inconsistent use of Place of Service (POS) codes and modifiers. Many payers require specific POS codes (such as POS 02 or POS 10) and modifier 95 to identify telehealth services. Incorrect coding or missing modifiers often results in claim rejections or denials.
Coverage policies for teletherapy CPT codes vary widely across payers, with some insurers limiting reimbursement for specific therapy durations or asynchronous services. Additionally, synchronous and asynchronous telehealth services are treated differently, requiring detailed documentation and payer-specific coding protocols.
These inconsistencies make it challenging for billing teams to submit clean claims, leading to extended AR cycles and administrative burden. Practices that fail to standardize telehealth billing workflows risk significant revenue delays.
2. Prior Authorization Delays and AI-Driven Utilization Management
Prior authorization requirements have expanded significantly in behavioral health billing, particularly for therapy sessions, residential treatment programs, and medication management services. In 2026, many payers use AI-driven utilization management systems to evaluate medical necessity and approve services.
While automation improves compliance, it also slows approval timelines. Authorization requests may take several days or weeks to process, and expired or missing authorizations can place claims on hold. Claims submitted without valid authorization are often denied outright, requiring resubmission and appeals.
Delays in prior authorization directly extend AR days and disrupt cash flow. Behavioral health practices must proactively track authorization expiration dates and implement workflows to ensure approvals are obtained before services are rendered.
3. Inconsistent Payer Coverage for Psychiatry Services
Unlike other medical specialties, psychiatry lacks standardized coverage rules across payers. Each insurance company sets its own policies for therapy, medication management, and psychiatric evaluation reimbursement.
Differences in coverage criteria, documentation requirements, and coding rules increase the risk of denied or underpaid claims. Billing teams must continuously adapt workflows to align with payer-specific policies, which adds complexity and increases administrative workload.
Inconsistent coverage policies also reduce revenue predictability, making financial planning difficult for behavioral health practices.
4. Coding and Documentation Errors
Coding and documentation errors remain a major contributor to AR delays in behavioral health billing. Common issues include missing medical necessity justification, incomplete session notes, and vague clinical documentation that fails to meet payer requirements.
Denied claims require corrections, resubmissions, and appeals, significantly extending AR cycles. Practices that lack standardized documentation templates and coder training programs face higher denial rates and prolonged reimbursement timelines.
Emerging Trends in Behavioral Health AR Management in 2026
| Trend | Traditional Practice | Impact on AR | Best Practice |
|---|---|---|---|
| AI Billing Automation | Manual claim tracking | Slow payments, higher AR days | Use AI for denials and tracking |
| Telehealth Billing Growth | Manual telehealth coding | Claim rejections | Standardize telehealth rules |
| Mental Health Parity Compliance | Limited compliance focus | Missed reimbursements | Align claims with parity laws |
| High-Deductible Plans | Poor upfront collections | Higher patient balances | Collect payments upfront |
| Online Patient Payments | Paper billing | Delayed payments | Use patient portals |
| Outsourced AR Services | Limited in-house staff | Slow AR recovery | Outsource to RCM experts |
| EHR-Billing Integration | Disconnected systems | Coding errors and delays | Use integrated platforms |
Key AR Metrics Behavioral Health Practices Must Track in 2026
Tracking the right AR metrics is crucial for improving cash flow and reducing AR days. Below are the key metrics every behavioral health practice should monitor:
Key AR Metrics (MGMA-Style Benchmarks)
| Metric | 2026 Benchmark | Goal |
|---|---|---|
| Average AR Days | 30–45 days | Reduce below 45 |
| AR Aging >90 Days | <10% of total AR | Minimize delayed payments |
| Clean Claim Rate | 90%+ | Reduce rework |
| Denial Rate by Payer | <5% | Track patterns |
| First-Pass Resolution Rate | 85–90% | Maximize efficiency |
| Patient Responsibility Collection | 80–95% | Improve upfront collections |
| Authorization-Related AR | <10% | Proactively manage approvals |
Best Practices to Reduce Behavioral Health AR Days in 2026
Reducing AR days in 2026 requires adopting best practices that streamline billing and improve collections. Here are the most effective strategies:
1. Clean Claim Submission
Ensure that all claims are submitted with accurate CPT/ICD-10 codes, modifiers, and complete documentation. The more accurate the claim, the less likely it is to be delayed or denied.
2. Telehealth Compliance Protocol
Standardize telehealth claims by applying the correct POS codes and modifier 95 for each payer. Ensure that your documentation clearly reflects the synchronous nature of the service to meet payer requirements.
3. Proactive Authorization Management
Track prior authorization expiration dates and submit renewals before the expiration period to ensure that claims aren’t delayed due to missing or expired authorizations.
4. Daily Denial Monitoring
Address denials within 24-48 hours to avoid aging claims. Quick action helps prevent delays in payments and reduces the time spent chasing payments.
5. Segment AR for Prioritization
Focus on high-dollar claims and those sitting in the 90+ days bucket. This helps prioritize resources and accelerates revenue recovery.
6. Monthly AR Review Meetings
Meet regularly with your billing team to review AR trends, payer patterns, and claim rejections. This ensures that you catch any issues early and resolve them efficiently.
7. Patient Responsibility Strategy
Collect co-pays and deductibles at the point of service. For high-deductible patients, offer payment plans and ensure that balances are paid faster.
How Cloud RCM Solution Helps Behavioral Health Practices Reduce AR Days
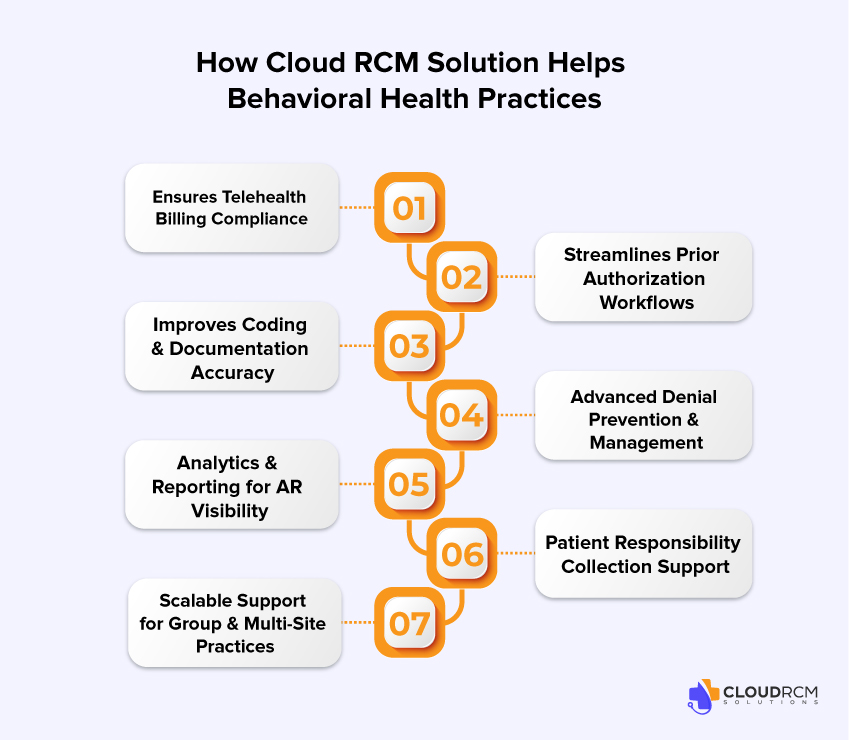
Cloud RCM Solution provides a comprehensive revenue cycle management platform designed to address the unique billing challenges of behavioral health practices. The platform ensures telehealth billing compliance by automatically applying correct POS codes and modifiers based on payer guidelines.
Cloud RCM Solution streamlines prior authorization workflows by tracking approval statuses in real time and alerting billing teams before authorizations expire. Expert coding support ensures accurate claim submission, while denial prevention tools identify root causes and prevent repeat errors.
Advanced analytics dashboards provide visibility into AR metrics, denial trends, and payer performance, enabling data-driven decision-making. Patient responsibility tools improve upfront collections and streamline patient billing communication.
Cloud RCM Solution is scalable for group practices and multi-site organizations, centralizing billing operations and standardizing workflows across locations.
Conclusion
In 2026, effectively managing AR days is critical for the financial stability and growth of behavioral health practices. Telehealth billing complexity, prior authorization delays, inconsistent payer coverage, and documentation errors pose significant challenges to revenue cycle performance.
By adopting best practices, tracking key AR metrics, and leveraging advanced RCM technology, behavioral health practices can streamline billing workflows, reduce denials, and accelerate reimbursements. Cloud RCM Solution offers a comprehensive platform to optimize revenue cycle performance and ensure sustainable financial growth. Schedule a free consultation today to see how our experts can reduce your AR days and maximize revenue.
FAQ’s
What is a good AR days benchmark for behavioral health practices?
A good benchmark is 30-45 days. Anything above 60 days indicates inefficiencies in billing or collections workflows.
Why are telehealth mental health claims frequently denied?
Telehealth claims are often denied due to incorrect POS codes, missing modifier 95, inadequate documentation, or payer-specific telehealth coverage restrictions.
How long does prior authorization take in psychiatry?
Prior authorization can take several days to weeks, depending on the payer, service type, and medical necessity documentation.
How can behavioral health practices reduce AR days?
Practices can reduce AR days by submitting clean claims, tracking prior authorizations, monitoring denials daily, segmenting AR, and improving patient collections.
Are telehealth claims more likely to be denied than in-person visits?
Yes, telehealth claims have higher denial rates due to evolving payer policies, documentation requirements, and coding complexities.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine