As the healthcare landscape evolves, independent providers face both exciting opportunities and tough challenges in delivering quality care while staying financially stable. Did you know that over 65 million Americans rely on Medicare, and Medicaid covers more than 82 million? These programs are crucial to the U.S. healthcare system and present a massive opportunity for independent providers to grow their practices. However, the process of Medicare & Medicaid Credentialing can be complex and time-consuming.
Here, we’ll explore the importance of Medicare & Medicaid Credentialing for Independent Providers, its benefits, and the challenges providers face when dealing with these systems.
Understanding Medicare & Medicaid Credentialing
Credentialing is the process through which healthcare providers like physicians and other healthcare practitioners, are verified by insurance companies, such as Medicare and Medicaid. It ensures that providers meet necessary regulations and standards before they are allowed to treat eligible patients and receive reimbursement for services provided.
For detailed insights on the credentialing process for both Medicare and Medicaid, check out our Medicare Credentialing and Medicaid Credentialing articles, where we explore the intricacies in more detail.
Medicare & Medicaid Eligibility Criteria:
| Criteria | Medicare | Medicaid |
| Age | 65 years or older | No age limit |
| Disability | Under 65 with 24 months of SSDI or ALS | Varies by state; typically for individuals with disabilities |
| Health Condition | ESRD or ALS | Long-term care or specialized medical needs |
| Income Level | No income requirement | State-specific income thresholds (based on FPL) |
| Residency | Must be a U.S. citizen or legal resident | Must reside in the state providing benefits |
| Medicaid Expansion | N/A | Covers adults up to 138% FPL in expansion |
Step-by-Step Guide for Credentialing Process
- Determine Eligibility: Before you start, ensure that your practice meets the basic requirements to participate in Medicare or Medicaid, such as licensing, board certifications, and malpractice insurance.
- Gather Required Documentation: Prepare essential documents, including proof of credentials, personal identification, and tax information. Be sure to check the specific documentation requirements for each state (for Medicaid).
- Submit an Application: For Medicare, providers can apply through the Medicare Provider Enrollment, Chain, and Ownership System (PECOS). For Medicaid, the application will depend on the state, so consult your state’s Medicaid website for the correct portal.
- Wait for Review and Approval: This process can take several months. During this time, the insurance company (Medicare or Medicaid) will review your application to verify that all credentials meet their standards.
- Ongoing Compliance: Once approved, you’ll need to maintain your credentials and renew them periodically. Be aware of any audits or follow-up requests to ensure continued eligibility.
Medicare Credentialing:
Medicare is the cornerstone of healthcare for millions of older Americans and individuals with certain disabilities. With more than 20% of the nation’s healthcare expenditures allocated to Medicare, participating in the program offers several advantages for independent practices.
Medicare Advantage (MA):
Medicare Advantage (MA) is a rapidly growing program where private insurance companies offer Medicare benefits with additional services. In 2025, an estimated 40% of Medicare beneficiaries are expected to enrol in MA, providing independent providers an opportunity to expand their patient base.
Providers interested in Medicare Advantage must submit their credentialing information through the Centers for Medicare & Medicaid Services (CMS). Once accepted, they benefit from faster payments, reduced administrative burdens, and predictable revenue.
The Benefits of Medicare for Independent Practices
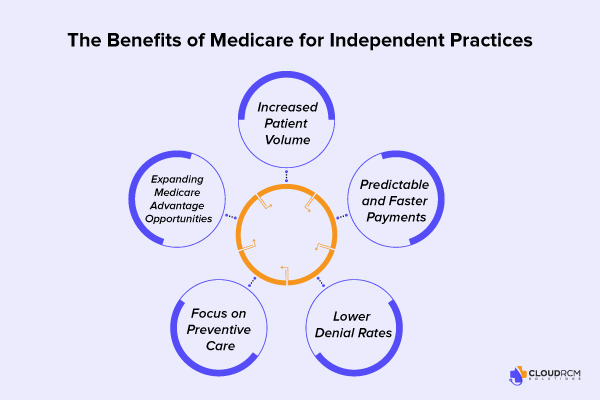
1. Increased Patient Volume
One of the most compelling reasons to accept Medicare is the potential for increased patient intake. According to recent CMS data, over 65 million Americans are enrolled in Medicare, providing a vast patient pool for independent practices. Younger physicians often find Medicare beneficial as they build their patient base.
2. Predictable and Faster Payments
Unlike many private insurers, Medicare offers transparent fee schedules and predictable payment cycles. Frank Cohen, Director of Analytics at Doctors Management, LLC, emphasizes that Medicare may not provide the highest reimbursement but compensates with faster payments and fewer administrative hassles.
3. Lower Denial Rates
Compared to commercial health plans, Medicare has lower denial rates, reducing the need for time-consuming appeals and resubmissions. This can alleviate administrative burdens and improve cash flow for independent practices.
4. Focus on Preventive Care
Medicare Advantage (MA) plans, in particular, prioritize preventive care and chronic disease management. This model not only improves patient outcomes but also aligns with value-based care initiatives. A study published in the American Journal of Managed Care highlighted a 32.8% reduction in the hazard of death for patients managed under risk adjustment programs.
5. Expanding Medicare Advantage Opportunities
Medicare Advantage has seen substantial growth, with projections indicating that MA enrollees will make up 40% of all Medicare patients by 2025. The program offers additional benefits like medication assistance, transportation, and disease management, making it attractive for both patients and providers.
Medicaid Credentialing:
Medicaid provides healthcare coverage for millions of low-income individuals, children, seniors, and those with disabilities. In 2024, Medicaid expansion enrollment reached 21.3 million people. Despite the unwinding of the continuous enrollment provision, which remained in effect until March 2024, the total enrollment in Medicaid expansion is still higher than it was in 2020.
State-Specific Medicaid Requirements
Unlike Medicare, Medicaid operates at the state level, meaning each state has its own process, requirements, and regulations for provider credentialing. Independent providers must be familiar with the specific guidelines in their state to ensure compliance and eligibility for reimbursement.
Key Benefits of Medicaid Credentialing:
- Expanded Patient Base: Medicaid provides access to a large and diverse pool of patients, including those who require ongoing care.
- Sociodemographic Reach: Credentialing with Medicaid allows providers to serve a variety of demographics, including children and elderly patients in need of care.
- Improved Public Health: By participating in Medicaid, providers contribute to expanding healthcare access for underinsured and uninsured populations, which improves overall public health outcomes.
The Challenges of Credentialing with Medicare & Medicaid
While the benefits of CMS Credentialing for Independent Providers are significant, there are also several challenges providers face in working with Medicare and Medicaid.
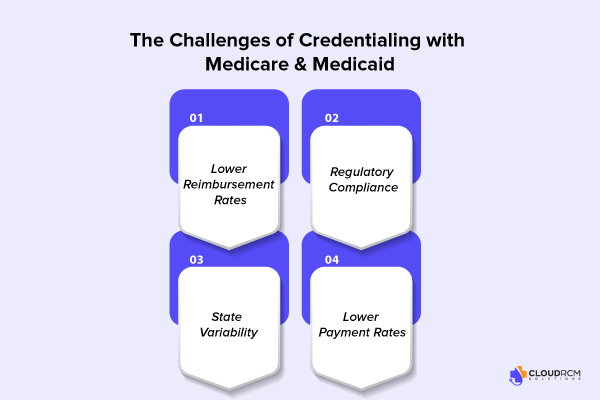
- Lower Reimbursement Rates: Medicare reimbursement rates are generally lower than those of commercial insurers, which may be a financial strain for some practices.
- Regulatory Compliance: Providers must adhere to a wide range of CMS regulations, including periodic audits, quality measures, and patient outcome reports.
- State Variability: Medicaid rules and regulations can vary widely by state, making it a challenge for multi-state providers to remain compliant across different regions.
- Lower Payment Rates: Like Medicare, Medicaid typically offers lower reimbursement rates compared to private insurance, making it crucial for practices to evaluate whether accepting Medicaid aligns with their financial goals.
Common Mistakes to Avoid in Credentialing
The credentialing process is thorough, and even small mistakes can lead to delays or denials. Here are common mistakes to avoid:
- Incomplete or Incorrect Documentation
- Failure to Keep Records Updated
- Not Understanding State-Specific Rules (for Medicaid)
- Delaying Submission
Medicare and Medicaid for Practice Growth
Despite the challenges, Medicare and Medicaid offer significant opportunities for independent providers. Medicare & Medicaid Credentialing for Independent Providers can foster long-term growth by expanding a practice’s patient base and creating more reliable revenue streams.
Focus on Value-Based Care:
Both Medicare Advantage and Medicaid programs increasingly focus on value-based care, rewarding providers for improving patient outcomes rather than the number of services rendered. Participating in these programs allows providers to earn additional incentives for improving chronic disease management, preventing hospital readmissions, and adhering to care protocols.
A study published in the American Journal of Managed Care found that patients enrolled in risk-adjusted programs like Medicare Advantage experienced a 6% increase in survival and a 32.8% lower hazard of death compared to those under traditional fee-for-service models. This proves that participating in value-based care programs ultimately benefits both the provider and the patient.
Reduced Administrative Burden:
Medicare’s processes, including lower denial rates and quicker payment cycles, make it easier for providers to manage the financial aspects of their practice. Medicaid’s reduced administrative burden, due to its lower denial rates and less frequent audits compared to private insurers, helps make it an efficient program for independent practices.
Medicare vs. Medicaid: Key Differences
| Category | Medicare | Medicaid |
| Purpose | For seniors (65+) and individuals with disabilities. | For low-income individuals and families. |
| Funding | Federally funded | Jointly funded by federal and state governments. |
| Eligibility | Age (65+) or qualifying disabilities | Income-based, varies by state. |
| Costs | Requires premiums, deductibles, and copayments. | Typically free or low-cost. |
| Coverage | Basic healthcare and prescription drugs. | Comprehensive, including long-term care. |
| Administration | Managed federally by CMS. | Administered at the state level. |
| Enrollment | Apply via Social Security or CMS. | Apply through state Medicaid offices. |
| Extras | Some plans (e.g., Medicare Advantage) offer extras like dental & wellness. | Includes dental, vision, and behavioural health. |
Tips for Finding the Best Medicare & Medicaid Advantage Plan
- Assess Your Health Needs: Choose a plan that covers your medical conditions, prescriptions, and preferred doctors.
- Understand Coverage Options: Ensure the plan offers additional benefits like dental, vision, and wellness programs if needed.
- Review Provider Networks: Confirm your doctors are in-network to avoid higher out-of-pocket costs.
- Compare Costs: Look beyond premiums—consider deductibles, copays, and out-of-pocket maximums.
- Check Prescription Drug Coverage: Ensure the plan covers your medications and offers the best prescription benefits.
- Look for Extra Benefits: Check for additional perks like gym memberships or transportation assistance.
- Consider the Plan’s Star Rating: Higher ratings indicate better customer satisfaction and care quality.
- Read Plan Reviews: Get insights from current enrollees about the plan’s performance and service.
Upcoming Changes or Policy Updates in Medicare & Medicaid
It’s important to stay informed about upcoming changes that may affect your credentialing or reimbursement processes. Some recent or upcoming changes to keep in mind include:
- Medicare Advantage Expansion: Medicare Advantage is expected to grow significantly in 2025, with enrollment projected to reach 40% of Medicare beneficiaries. This will increase opportunities for independent providers to tap into a larger patient pool.
- Medicaid Expansion: More states are expanding Medicaid eligibility in 2024, which could increase the number of patients eligible for care. However, each state has different rules, so staying up-to-date with state-specific guidelines is critical.
- Payment Rate Adjustments: Both Medicare and Medicaid regularly adjust payment rates. These changes can impact your revenue cycle, so it’s important to monitor updates from CMS and your state Medicaid office.
Final Thought:
Medicare & Medicaid Credentialing for Independent Providers is a vital step for independent providers looking to expand their reach, grow their practice, and improve patient outcomes. While the credentialing process can be complex, the benefits far outweigh the challenges. By gaining access to a larger patient base, increasing reimbursement predictability, and participating in value-based care, independent providers can ensure their practice’s success in an increasingly competitive healthcare environment.
Understanding the requirements, staying compliant, and embracing the opportunities presented by these programs will help providers offer better care to more patients while achieving financial stability and growth.
Why Choose CloudRCM Solutions?
CloudRCM Solutions simplifies Medicare and Medicaid credentialing, helping independent providers save time and reduce administrative burdens. Our expert team ensures compliance, accelerates reimbursement cycles, and provides the tools you need to focus on patient care. Partner with us to streamline your credentialing process and grow your practice with confidence.
Don’t let Medicare and Medicaid credentialing complexities slow you down. Schedule an appointment today call us at (224) 231-6880 for a free consultation, and get credentialed with ease.
FAQs
What does it mean to be Medicaid credentialed?
It means you have been verified to meet the requirements to treat Medicaid patients and receive reimbursements.
How do I become an independent Medicare provider?
Submit an application through PECOS, provide the necessary documentation, and complete the review process.
How do I bill Medicaid as a provider?
Submit claims through your state’s Medicaid billing portal after becoming a credentialed provider.
Can a provider have more than one Medicaid ID?
Yes, providers may have different IDs for multiple states or practice locations.
How often does Medicare require credentialing?
Credentialing must be renewed every 3-5 years depending on the Medicare plan requirements.
Does Medicare use CAQH for credentialing?
No, Medicare requires providers to use PECOS for credentialing instead of CAQH.
Are providers required to accept Medicare?
No, accepting Medicare is optional for healthcare providers.
Does Medicare require board certification?
No, board certification is not mandatory, but providers must meet state licensing and credentialing

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine