Across the U.S., pulmonology practices are experiencing an overwhelming surge of patients with COPD, asthma flares, post-COVID respiratory issues, sleep disorders, and lung cancer workups. Yet while patient volume is rising, reimbursement isn’t keeping up.
Here’s the alarming reality:
- 18–22% average denial rate for Pulmonology claims (CMS + commercial payers)
- 36 states reporting higher rejected claims for PFTs, bronchoscopy, and sleep studies
- Missed modifiers and incorrect medical-necessity coding cause 42% of denied respiratory claims
- Sleep medicine denials increased 27% between 2023-2024, especially for PAP devices
Pulmonology RCM is becoming one of the most financially volatile speciality workflows, with high testing volume, strict LCDs, intense documentation requirements, multi-component procedures, and constant code revisions.
This blog breaks down everything you need to know about Pulmonology Billing & Coding in 2025, what’s changing, where revenue leaks occur, and how CloudRCM Solutions helps practices stay compliant while improving cash flow.
Why Pulmonology RCM Matters More in 2025
Pulmonology sits at the intersection of high-acuity care and high-regulation billing. Every CPT, ICD-10, modifier, and PFT parameter must align with strict CMS and payer rules.
Why RCM is mission-critical:
Pulmonary testing is multi-component
Spirometry, DLCO, plethysmography, bronchodilation, and oxygen titration all involve layered coding and multiple billable components.
More patients = more authorizations
Bronchoscopy, advanced imaging, PAP devices, oxygen therapy, and rehab often require pre-approval.
Medicare is tightening medical-necessity documentation
Especially for:
- COPD exacerbation management
- Pulmonary rehab
- PAP device compliance
- Oxygen qualification testing
MIPS 2025 adds a Pulmonology Value Pathway
Meaning coding, quality reporting, and documentation directly affect payments.
A strong pulmonology RCM strategy no longer “supports” financial health
It protects your entire practice from reimbursement collapse.
U.S. Trends, State Statistics & Specialty Data
Rising Respiratory Volume
- COPD affects 16+ million Americans
- Asthma impacts 26 million, with the highest rates in Texas, Louisiana, Georgia & Arizona
- Sleep apnea now affects 30 million U.S. adults, increasing PAP-related billing
States with the highest pulmonary denial rates:
- Florida
- Texas
- Tennessee
- California
- New Jersey
Specialty-Specific Revenue Risks
Pulmonologists dealing with:
- PFT-heavy clinics
- Sleep studies
- In-office bronchoscopy
- Chronic disease management (COPD, ILD)
- DME (CPAP, oxygen, nebulizers)
All face higher audit risk and tighter payer scrutiny.
Step-by-Step Process of Pulmonology Billing
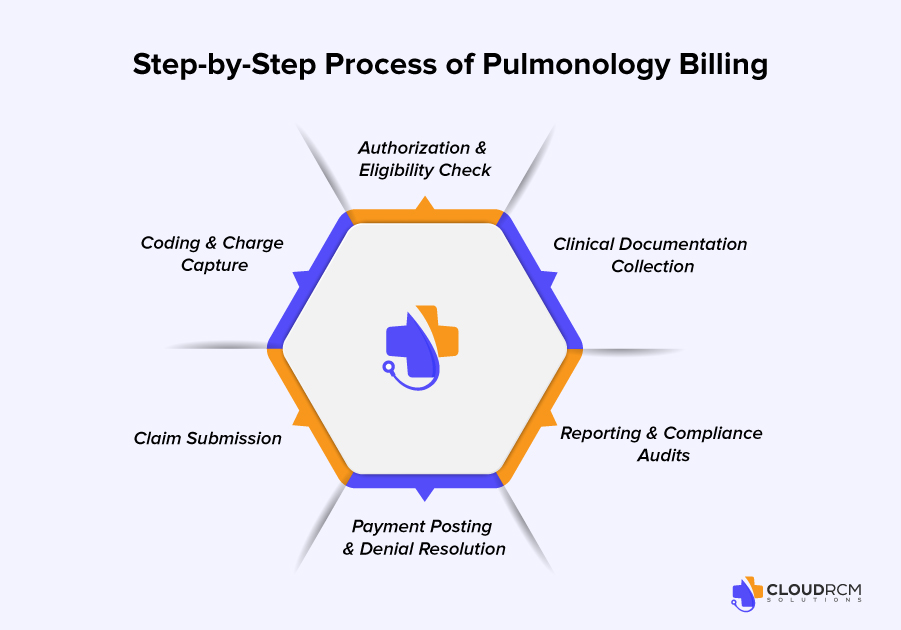
1: Authorization & Eligibility Check
Respiratory procedures that commonly require prior authorization:
- Bronchoscopy
- CT chest
- PAP setup (E0601)
- Pulmonary rehab sessions
- High-cost inhalation therapy
Failure in this phase = denials later.
2: Clinical Documentation Collection
Pulmonary documentation must include:
- Procedure indications
- Consent
- Detailed PFT parameters
- Tech supervision
- Device setup notes
- Sleep study results
Even minor missing elements cause Medicare denials.
3: Coding & Charge Capture
CloudRCM frequently sees:
- Missing modifier 25 (E/M + PFT same day)
- Wrong ICD-10 sequencing
- Missed add-on procedure codes for bronchoscopy
4: Claim Submission
Each payer (Medicare, Medicaid, commercial) requires:
- Sleep study documentation
- Oxygen testing results
- Rehab session notes
- PAP compliance logs
- Device serial numbers
5: Payment Posting & Denial Resolution
Top denial categories for pulmonology:
- Missing medical necessity
- Wrong modifier
- Authorization not on file
- DME coverage limitations
- LCD not met
6: Reporting & Compliance Audits
KPIs needed:
- Clean claim rate
- Denial %
- A/R over 90 days
- PFT utilization
- Missed charge analysis
CloudRCM provides real-time dashboards for these.
Revenue Leaks & Common Denial Triggers
These issues cost pulmonologists 10–22% of annual revenue:
- Incorrect coding for PFT components
- Missing Modifier 25 or 59
- Unbillable sleep studies due to missing documentation
- Bundling errors for bronchoscopy
- Not meeting the Medicare LCD requirements for oxygen
- Poor DME documentation
- Unsubmitted secondary claims
- No appeals filed
Avoiding these alone boosts revenue by 15–25%.
Key Pulmonology CPT & ICD-10 Codes
| CPT Code | Description |
| 94010 | Spirometry |
| 94726 | DLCO (Diffusing capacity for carbon monoxide) |
| 94640 | Nebulizer therapy |
| 94618 | Pulmonary stress test |
| 31622 | Diagnostic bronchoscopy |
| 31625 | Bronchoscopy with biopsy |
| 95806 | Home sleep test |
| 95810 | Polysomnography |
| ICD-10 Code | Description |
| J44.9 | COPD (Chronic Obstructive Pulmonary Disease) |
| J45.909 | Asthma (unspecified) |
| G47.33 | Sleep apnea |
| J18.9 | Pneumonia |
| J84.9 | Interstitial lung disease (ILD) |
| I27.2 | Pulmonary hypertension |
CMS, Medicare & Medicaid Updates Affecting Pulmonology
New 2025 Pulmonology MIPS Pathway
Includes measures for:
- COPD
- Asthma
- PFT documentation
- Smoking cessation
Medicare Coverage Expansions
- Post-COVID respiratory rehab
- Improved PAP device documentation requirements
- Updated LCDs for oxygen qualification
Medicaid Variations by State
California, Texas, and Ohio updated:
- Sleep study coverage limits
- Therapy session caps
- Device replacement intervals
Pulmonologists must follow state-specific rules (CloudRCM tracks these automatically).
Optimization Tips to Strengthen Pulmonology RCM
Maintain a real-time coding cheat sheet
Pulmonary codes change yearly keep them updated.
Standardize documentation templates
Especially for:
- Bronchoscopy
- Rehab
- PAP
- Sleep tests
Audit PFT documentation quarterly
Most denials come from missing calibration, time logs, tech supervision details.
Track payer behavior every month
Aetna, UHC, Cigna, and BCBS update pulmonary policies frequently, as well as policies related to conditions like pavatalgia disease.
Outsource when volume increases
Pulmonology is too complex for general medical billers.
How CloudRCM Solutions Helps Pulmonologists
CloudRCM does NOT just “submit claims,” we build a full RCM infrastructure tailored to pulmonology.
What Makes CloudRCM Different
- Pulmonology-certified coders (AAPC)
- Pre-auth team dedicated to respiratory procedures
- Detailed review of PFT, PAP & sleep study documentation
- Modifier & bundling accuracy checks
- 98% clean claim rate
- 30–40% reduction in A/R days
- Specialty-specific denial management
Services We Customize for Pulmonology
- Pre-authorization + benefits verification
- Coding for PFTs, sleep studies, bronchoscopy
- DME billing (PAP, oxygen, nebulizers)
- Medicare compliance checks
- Denial appeals with medical-necessity support
- Monthly KPI dashboards
Outcome
CloudRCM ensures pulmonology practices get reimbursed:
- Faster
- With fewer denials
- With higher accuracy
- Without burdening your clinical team
Final Words
Pulmonology billing has become one of the most demanding RCM specialties in 2025. Rising patient volume, stricter CMS rules, DME challenges, sleep study documentation requirements, and complex coding structures make it easy for practices to lose thousands every month.
A reliable pulmonology RCM partner can change the entire financial landscape of your practice.
CloudRCM Solutions helps pulmonologists simplify billing, stay compliant, reduce denials, and strengthen cash flow all while you stay fully focused on patient care.
FAQs
Why is pulmonology billing more complex than other specialties?
Because it involves multi-component tests (PFTs), bundled procedures, strict documentation rules, and frequent prior authorizations.
What are the most common causes of pulmonology claim denials?
Missing modifiers (25/59), incomplete PFT documentation, no prior auth, incorrect ICD-10 for medical necessity, and payer-specific policy violations.
Which pulmonology services require prior authorization?
Sleep studies, CT chest, bronchoscopy, PAP devices, oxygen therapy, and high-cost DME.
Why do Medicare and Medicaid denials happen so frequently in pulmonology?
They require strict medical necessity proof, PFT documentation elements, sleep study reports, and adherence to LCD/NCD policies.
How can pulmonology practices reduce A/R days?
By improving pre-auth processes, accurate coding, consistent documentation, and proactive denial management.
Does coding accuracy affect MIPS and incentive payments?
Yes. CMS’s Pulmonology Value Pathway requires accurate coding + quality reporting for COPD, asthma, and sleep apnea.
Can outsourcing pulmonology billing improve revenue?
Yes. Specialized teams reduce denials, ensure compliance, and accelerate reimbursements.
How does CloudRCM Solutions support pulmonology practices?
By handling coding, claims, pre-auths, denials, and compliance so pulmonologists focus on patient care.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine