Over 20% of U.S. adults live with a mental illness, yet only about half receive treatment, and limited access to in-network providers is a big reason why. Meanwhile, therapists report credentialing wait times ranging from 1 to 3 months, and in some cases stretching to 4–6 months, depending on the payer and documentation speed.
If that makes you think, “No wonder it’s daunting,” you’re not alone, and with the right strategy, credentialing can become your path to stability rather than a roadblock.
What Is Mental Health Provider Credentialing?
Mental health credentialing, also called insurance credentialing for therapists, counselors, and other providers, is the process insurers use to verify your qualifications before listing you as an in-network provider. This includes checking your license, education, malpractice coverage, NPI, and CAQH profile. Once credentialed, you can accept insurance, expand your client base, and make care more affordable for the patients who need you most.
How to get credentialed as a mental health provider
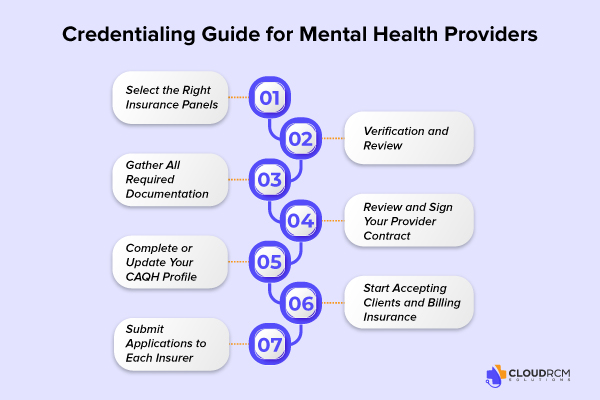
Getting credentialed with insurance companies can feel overwhelming, but breaking it into simple steps makes the process manageable. Here’s a clear path to becoming an in-network provider:
Select the Right Insurance Panels
Start by identifying insurers that align with your specialty, location, and target clients. Consider PPO vs. HMO networks, reimbursement rates, and patient volume to ensure your practice grows efficiently.
Gather All Required Documentation
Insurance companies typically request your state license, National Provider Identifier (NPI), malpractice insurance, CAQH ProView profile, W-9 form, and resume or CV. Having all documents organized in advance reduces delays and ensures your application is complete.
Complete or Update Your CAQH Profile
Most insurers use CAQH ProView to verify provider credentials. Ensure your information is accurate, verified, and up to date. Even minor errors can slow the credentialing timeline.
Submit Applications to Each Insurer
There’s no universal credentialing application, so submit separately to each insurance company. Carefully review their specific requirements to avoid mistakes that could cause delays.
Verification and Review
Insurers verify your education, licensure, work history, and background. This stage typically takes 90–150 days, though timelines vary by company and completeness of documentation.
Review and Sign Your Provider Contract
Once approved, you’ll receive a contract outlining reimbursement rates, billing policies, and obligations. Take time to review terms carefully to protect your practice.
Start Accepting Clients and Billing Insurance
After final approval, you’ll appear in insurance directories as an in-network mental health provider. You can now see insured clients, submit claims, and expand your reach within the community.
Credentialing Challenges for Mental Health Providers
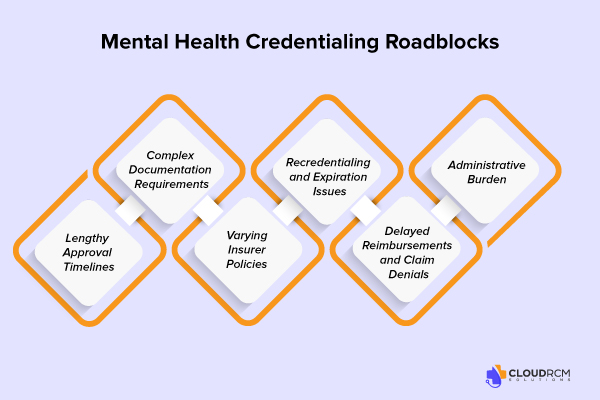
While becoming an in-network provider offers numerous benefits, mental health credentialing presents its own set of challenges. Understanding these hurdles can help therapists, counselors, and psychologists prepare and avoid common delays:
Lengthy Approval Timelines
Credentialing can take 90–150 days or more, depending on the insurer and the completeness of your application. Even small errors, missing documents, or delays in verification can stall the process.
Complex Documentation Requirements
Insurance companies require multiple forms of documentation, including licenses, NPI, W-9, malpractice coverage, and CAQH profiles. Keeping everything organized is critical; a single missing item can reset the application timeline.
Varying Insurer Policies
Each insurance company has different rules, application formats, and verification processes. Navigating multiple payer requirements can be confusing and time-consuming, especially for private practices managing a growing caseload.
Recredentialing and Expiration Issues
Credentialing isn’t a one-time event. Providers must regularly update their licenses, insurance policies, and CAQH profiles. Missing deadlines can result in temporary removal from insurance panels.
Delayed Reimbursements and Claim Denials
Even after credentialing, claims may be denied due to administrative errors, coding mistakes, or missing provider information. This can create financial strain for smaller practices.
Administrative Burden
Many therapists find the credentialing process overwhelming alongside clinical duties. Without dedicated staff or credentialing services, it’s easy to fall behind or make errors.
Overcoming Credentialing Challenges for Mental Health Providers
Credentialing can feel like a long, complicated process, but with the right approach, therapists and counselors can deal with it efficiently and stay in-network. Taking proactive steps reduces delays, minimizes stress, and helps your practice grow.
- Stay Organized: Track all documents, deadlines, and submissions.
- Use CAQH Proactively: Keep your profile updated and attested.
- Follow Up Regularly: Maintain communication with insurers.
- Consider Credentialing Services: Outsource paperwork to save time.
- Plan for Recredentialing: Keep licenses and insurance info current.
- Use Technology: Use software or reminders to improve the process.
Benefits of Being Credentialed for Mental Health Providers
Becoming credentialed with insurance companies isn’t just a bureaucratic requirement; it’s a strategic step that can transform your practice. Here’s why credentialing matters for therapists, counselors, and other mental health providers:
Increased Patient Base and Visibility
Once you’re listed as an in-network mental health provider, your practice becomes discoverable to thousands of patients actively searching for covered care. Patients are more likely to choose providers who accept their insurance, which can significantly expand your client base.
Easier Billing and Reimbursement
Credentialing simplifies claims submission and ensures smoother reimbursement. Being in-network means insurers recognize your credentials, reducing the risk of claim denials and delayed payments, so your practice maintains a more predictable revenue flow.
Boosted Credibility and Trust
Insurance panels verify your license, education, work history, and malpractice coverage, which can reassure patients and strengthen your professional reputation. Being credentialed signals that your practice is reliable, compliant, and committed to quality care.
Ability to Provide Affordable, Insurance-Covered Care
Many clients rely on their insurance to access mental health services. By becoming credentialed, you make your services more affordable and accessible, removing a common barrier to treatment and helping more people get the care they need.
Tips for Faster Mental Health Credentialing
Speeding up credentialing doesn’t have to be complicated. Follow these practical tips to get in-network faster:
- Double-Check Documentation: Ensure licenses, NPI, malpractice insurance, W-9, and CAQH profile are complete and accurate.
- Use CAQH Effectively: Keep your profile updated and attested to prevent delays.
- Maintain a Calendar: Track application submissions, follow-ups, and recredentialing deadlines to stay on top of every step.
Credentialing for Group Practices vs. Solo Practices
Credentialing can look different depending on whether you run a solo therapy practice or are part of a group practice. Understanding these differences helps you plan and avoid delays.
Solo Practices
- Each therapist applies individually to insurance panels.
- You are fully responsible for submitting all documentation and tracking approvals.
- Credentialing timelines can range from 1–3 months, depending on the insurer and the completeness of your application.
Group Practices
- The practice may hold a group contract with insurers, which can simplify credentialing for multiple providers.
- New providers often need to be added individually, but shared CAQH profiles and group NPIs can reduce paperwork.
- Managing multiple providers requires careful tracking of licenses, recredentialing deadlines, and provider directories to ensure everyone remains in-network.
Cost & Time Considerations for Mental Health Credentialing
Understanding the time and cost involved in mental health credentialing helps therapists plan effectively and avoid surprises:
- Time Investment: Credentialing typically takes 90–150 days, sometimes stretching to 4–6 months, depending on the insurer and documentation.
- Recredentialing: Providers must update licenses, insurance, and CAQH profiles every 2–3 years.
- Direct Costs: Usually minimal, but include document preparation and submission fees if applicable.
- Indirect Costs: Staff time, administrative work, and potential revenue delays can add up.
- Outsourcing Option: Credentialing services or billing partners can save time, reduce errors, and speed up approvals.
Final Thoughts
Mental health credentialing may feel complex, but it’s a crucial step toward growing a sustainable, in-network practice. By staying organized, keeping your CAQH profile updated, and following a clear process, therapists can reduce delays, avoid common mistakes, and focus on what matters most: providing quality care to clients. With the right strategy, credentialing becomes not a roadblock but a pathway to expanding your reach and strengthening your practice.
Simplify Your Credentialing with CloudRCM
Credentialing doesn’t have to be stressful. CloudRCM helps mental health providers get credentialed faster by managing applications, CAQH updates, and insurer follow-ups so you can focus on your patients, not paperwork.
Ready to get credentialed without the hassle? Partner with CloudRCM today.
FAQs
How do I get credentialed with insurance as a therapist?
Submit applications to each insurer with required documents, complete your CAQH profile, and follow up until verification is complete.
How long does CAQH credentialing take for mental health providers?
Typically, 2–6 weeks to verify your CAQH profile, but overall insurance credentialing can take 90–150 days.
Which documents do I need for insurance credentialing?
State license(s), NPI, malpractice insurance, CAQH ProView profile, W-9 form, and your resume or CV.
Why is my mental health credentialing taking so long?
Delays often occur due to missing documents, incomplete CAQH profiles, insurer-specific requirements, or slow verification processes.
Can I see clients before my insurance credentialing is approved?
You can see clients, but you cannot bill insurance until credentialing is complete.
What are the common mistakes that delay therapist credentialing?
Missing documents, outdated CAQH profiles, ignoring insurer requirements, and delayed follow-ups are the main pitfalls.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine