If you’re a provider who accepts Traditional Medicare, a major change is coming that could significantly affect your revenue, workflows, and patient care delivery.
The Centers for Medicare & Medicaid Services (CMS) is piloting a new model called WISeR short for Wasteful and Inappropriate Services Reduction, which introduces AI-powered prior authorizations into Traditional Medicare starting in 2026.
Until now, providers saw Medicare Advantage patients get hit with denials and delays due to automated pre-checks. But Traditional Medicare? It’s been largely free of those hurdles.
Not anymore.
What WISeR Means for You and Your Practice?
WISeR (Wasteful and Inappropriate Services Reduction) is CMS’s upcoming initiative to bring AI-powered prior authorizations into Traditional Medicare, something that, until now, mostly impacted Medicare Advantage plans.
WISeR uses algorithms to flag “low-value” services and either approve or deny them automatically, with vendors, not CMS staff, handling the tech. While CMS promises oversight, the shift raises red flags for providers.
Just look at Medicare Advantage: In 2023, nearly 50 million prior authorization requests were submitted, up from 42 million in 2022. Of those, 3.2 million (6.4%) were denied, but when appealed, 81.7% were overturned. Yet, only 11.7% of denials were even appealed, meaning most went unchallenged.
If WISeR mirrors this pattern, providers could face increased denials, delayed care, and greater admin burden, even for necessary services. This makes early preparation essential.
Read: Medicare Enrollment & CMS Credentialing Guide
What This Could Mean for Your Practice?
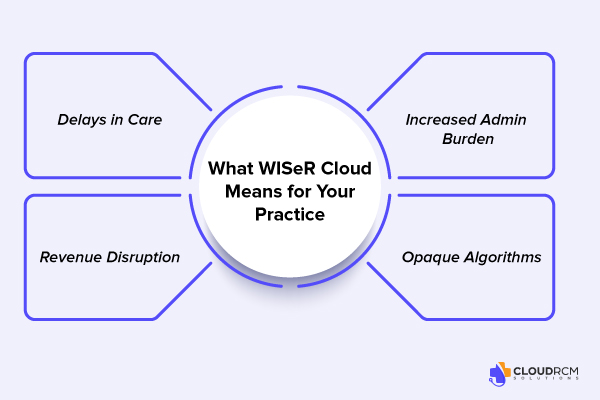
While CMS frames WISeR as a way to reduce waste, the practical reality for providers is more complicated. The rollout of AI-powered prior authorizations into Traditional Medicare brings a new layer of administrative complexity, and providers are right to be concerned.
Here are the four biggest risks to be aware of:
Delays in Care
Automated denials and added steps for approval can delay patient treatments, especially for time-sensitive services like diagnostics, imaging, or therapies. What once could be scheduled immediately may now require days or even weeks of back-and-forth.
Increased Admin Burden
Prior authorizations are time-consuming. Your team may soon be tied up with extra forms, portal logins, and payer phone calls, all of which pull staff away from front-desk operations and clinical support. That means longer wait times, reduced patient throughput, and more pressure on your admin staff.
Revenue Disruption
More denials mean more delayed or missed payments. If services are flagged or denied without warning, your practice could see serious cash flow interruptions, particularly dangerous for small to mid-sized practices with limited billing bandwidth.
Opaque Algorithms
Unlike human reviewers, AI systems don’t consider context or clinical nuance. They follow rigid logic that can trigger denials even when services are clearly necessary. Worse, the denial rationale may not be transparent, making appeals more difficult and time-consuming.
How Should Providers Prepare for WISeR?
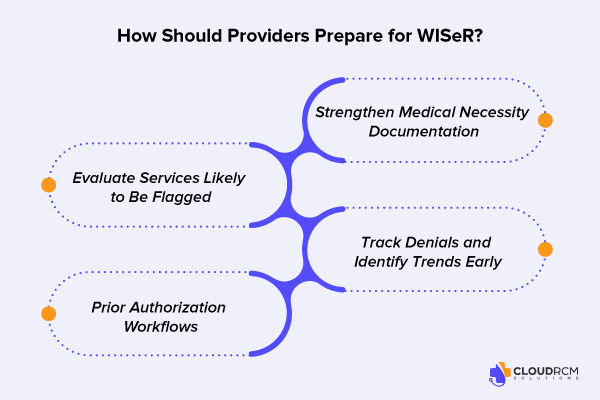
The introduction of WISeR represents more than just another policy update; it’s a fundamental shift in how care is authorized and reimbursed within Traditional Medicare. While CMS positions this as a move to eliminate waste and unnecessary services, the operational and financial impact on providers could be significant.
Rather than waiting for the rollout in 2026, providers can begin preparing now. Here’s what that might look like in practice:
Evaluate Services Likely to Be Flagged
Start by identifying procedures and services in your practice that may be considered “low-value” under CMS definitions. These often include:
- Advanced diagnostic imaging (MRI, CT scans)
- Pain management injections
- Certain orthopedic procedures
- DME and home health referrals
- Repetitive therapy sessions
Strengthen Medical Necessity Documentation
With AI algorithms determining approval, clinical nuance must be documented clearly and consistently. Providers should begin reviewing how medical necessity is recorded in their charts. Consider:
- Implementing templates for common services
- Training staff on what payers define as “sufficient documentation”
- Auditing current charts to identify potential gaps
Prior Authorization Workflows
Even if you haven’t had to deal with prior authorizations for Traditional Medicare in the past, that will likely change. Now is the time to:
- Assign clear ownership of prior auth tasks within your team
- Build a centralized process (not scattered across multiple roles)
- Prepare scripts and checklists to reduce back-and-forth with payers
Track Denials and Identify Trends Early
Don’t wait until denials become frequent. Implement a system to track and categorize any denials received under Medicare, even now. Look for:
- Denial reasons (medical necessity, missing auth, coding errors)
- Service types or CPT codes most affected
- Differences across payers or regions
How CloudRCM Prepares Your Practice for What’s Next
With major changes like WISeR on the horizon, providers shouldn’t have to choose between staying compliant and focusing on patient care. At CloudRCM, we make it our job to handle the administrative complexity so you can focus on what matters most: your patients.
Here’s how we support your practice in adapting to this new Medicare model:
Complete Prior Authorization Management
Our team monitors Medicare policy updates in real time and manages the entire prior authorization process on your behalf. From verifying eligibility and gathering clinical documentation to submitting requests and following up with payers, we take care of every step, reducing delays and administrative strain on your staff.
Coding Accuracy That Prevents Denials
We combine expert-level coding with smart technology to ensure that the claims are coded correctly and supported with proper documentation. This approach helps you to reduce the chances of denials and helps you maximize the clean claim rates, which means faster payment and fewer appeals.
WISeR Monitoring and Customized Alerts
As WISeR begins to roll out across Traditional Medicare, we closely track its implementation by region and specialty. We provide clear, concise updates and recommendations specific to your practice, no policy overload, just actionable information when you need it.
Strategic Denial Management and Appeals
If a claim is denied, especially by an AI-driven system, we step in with well-prepared appeals that align with CMS guidelines for medical necessity. Our team doesn’t just resubmit claims; we advocate for your services with evidence-based documentation to help recover lost revenue.
Final Thought:
WISeR signals a turning point for Traditional Medicare. In 2021, Medicare Advantage plans made over $ 35 million in prior authorization determinations, and over 2 million of these were denied. For decades, providers have operated with minimal pre-authorization barriers, but that’s about to change. As AI-driven decisions replace human review, the risk of delayed care, denied claims, and disrupted cash flow grows. Practices that proactively adapt their documentation, workflows, and denial strategies will be best positioned to protect both patients and revenue in this new environment.
Take Action with CloudRCM
Don’t let AI-driven denials catch your practice off guard. CloudRCM helps you get ahead of WISeR with proactive authorization workflows, expert coding support, and real-time monitoring. Ready to protect your revenue and reduce admin overload? Contact CloudRCM today and let us help you deal with Medicare’s next big shift before it impacts your bottom line.
FAQs
What services will WISeR target first?
CMS has not released a full list yet, but early indicators suggest WISeR will focus on high-cost or frequently overused services. These may include advanced imaging (CT, MRI), repetitive therapy, certain orthopedic procedures, and DME/home health referrals.
Does WISeR affect PECOS enrollment?
Not directly, PECOS (Provider Enrollment, Chain, and Ownership System) is used for enrolling in Medicare, while WISeR governs how services are authorized. However, up-to-date PECOS enrollment is required for providers to bill Medicare and receive prior auth decisions under WISeR.
Will all Medicare providers need to submit prior authorizations in 2026?
Only providers in regions or specialties selected for the WISeR pilot will be required to submit prior authorizations initially. However, CMS may expand the program nationwide depending on outcomes.
Is WISeR replacing Medicare Advantage authorization rules?
No. WISeR applies only to Traditional Medicare. Medicare Advantage plans will continue using their own prior authorization processes, separate from WISeR.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine