Behavioral health and psychiatry practices are facing significant billing challenges in 2026. With telehealth continuing as a core service, stricter payer policies, and frequent prior authorizations, Accounts Receivable (AR) days are on the rise. AR cycles extending to 60, 90, or even 120+ days are creating a financial strain, disrupting cash flow, and impeding growth for these vital practices.
Reducing AR days is no longer just a financial goal; it’s essential for the sustainability of your practice. In this blog, we’ll explore the top AR challenges in behavioral health and provide practical solutions to optimize your revenue cycle performance. We’ll also demonstrate how Cloud RCM Solution can support your practice in reducing AR days and improving financial health.
What Accounts Receivable (AR) Means for Behavioral Health Practices in 2026
Accounts Receivable (AR) refers to the money your practice is owed by payers, including commercial insurance, Medicare, Medicaid, and patients. The key metric for measuring AR efficiency is AR days, the number of days between the date a service is provided and when payment is received.
Why AR Matters:
- Cash Flow: Extended AR days slow down your incoming revenue, affecting daily operations, payroll, and investments in technology and growth.
- Profitability: High AR days indicate inefficiencies in your billing processes, leading to increased administrative costs and lost revenue.
- Operational Impact: The more time your staff spends chasing unpaid claims, the less time they have to focus on delivering quality care to your patients.
Top AR Challenges in Behavioral Health / Psychiatry (2026)

1. Telehealth Billing Requirements Are Complex
Telehealth has become a cornerstone of mental health care in 2026. However, it comes with its own set of billing challenges. Inaccurate Place of Service (POS) codes and modifier 95 usage are common causes of denied telehealth claims.
Challenges:
- POS Codes & Modifier 95: Different payers have different rules for telehealth, making it easy to miss the right POS code or modifier.
- Teletherapy CPT Codes: Some payers have reduced coverage for specific teletherapy CPT codes, leading to confusion and denial.
- Inconsistent Coverage: Synchronous and asynchronous services are treated differently across payers.
Impact on AR: Misapplied codes or non-compliant billing practices can lead to claim rejections or delayed payments, extending AR days and disrupting cash flow.
2. Increased Prior Authorization Delays
Prior authorization is a significant part of the billing process in behavioral health, but it introduces delays. Services like therapy sessions, medication management, and residential treatments now require frequent authorization.
Challenges:
- Stricter Authorization Criteria: Insurers use AI-driven tools to validate medical necessity, which can slow down approval timelines.
- Long Processing Times: The process for prior authorization can take days or even weeks, putting a strain on cash flow.
- Authorization Expirations: Missing or expired authorizations can result in claims being put on hold, further delaying revenue collection.
Impact on AR: Without proper authorization in place, claims sit in pending status, prolonging AR cycles and pushing payments into the future.
3. Inconsistent Payer Coverage for Psychiatry Services
Unlike other specialties, there is no universal billing standard for psychiatric services. Each payer has different rules for covering therapy codes, medication management, and psychiatric evaluations.
Challenges:
- Different Coding Requirements: Payers vary in how they reimburse therapy codes, medication management, and Evaluation and Management (E/M) codes, leading to confusion.
- Misaligned Coverage: Some payers may refuse reimbursement for certain procedures or services, leaving practices with unpaid claims.
Impact on AR: Misalignment with payer policies leads to underpaid or denied claims, which further increase AR days and delay payments.
4. Coding & Documentation Errors Still Drive Denials
Even routine therapy sessions can face denials if the documentation does not adequately support the billed codes.
Common Documentation Gaps:
- Missing Medical Necessity: Claims without a clear justification for the service provided are likely to be denied.
- Incomplete Session Notes: Payors require thorough session notes that are linked to the diagnosis to process claims.
- Non-specific Clinical Records: Vague or incomplete clinical records lead to issues with payer reviews.
Impact on AR: Denied claims must go through the appeals process, which can extend AR days, resulting in longer delays in receiving payments.
Emerging Trends in Behavioral Health AR Management vs. Traditional Practices in 2026
| Emerging Trend | Traditional Practices | Impact on AR | Best Practice/Approach |
| Integration of AI and Automation in Billing | Manual claims tracking and denials management. | Slower claim resolution, higher AR days due to manual errors. | Leverage AI tools to automate claim tracking, detect errors, and predict denials. |
| Telehealth Expansion and Integration | Telehealth claims handled manually without standardized protocols. | Increased rejections due to inconsistent coding and modifiers. | Automate telehealth claims with preset rules for coding and modifiers. |
| Behavioral Health Parity Act Compliance | Less focus on compliance with mental health parity laws. | Missed reimbursements for mental health services under parity rules. | Ensure all mental health claims are in compliance with Mental Health Parity laws. |
| Increased Use of High-Deductible Health Plans (HDHPs) | Collecting co-pays at point of service is inconsistent. | Increased patient balances, delayed payments, and higher AR days. | Implement upfront patient responsibility collection and offer payment plans. |
| Value-Based Care Payment Models | Fee-for-service billing without considering patient outcomes. | Claims based on volume, not value, leading to lower reimbursement. | Adopt value-based care models, focusing on patient outcomes and bundled payments. |
| Telehealth Compliance and Reimbursement Complexity | Telehealth reimbursement challenges due to unclear regulations. | Telehealth claims denied or underpaid due to non-compliant coding. | Standardize telehealth documentation, POS codes, and ensure payer-specific compliance. |
| Patient Payment Portals and Online Bill Pay | Traditional paper billing and phone collections. | Longer AR days due to delayed checks and mailed payments. | Integrate online payment systems and patient portals for easier and faster payments. |
| Outsourcing AR Management and Billing Services | In-house billing with limited resources. | High operational cost, slow AR recovery, and staff burnout. | Outsource AR management to specialized services to reduce overhead and improve efficiency. |
| Interoperability Between EHR and Billing Systems | Disconnected EHR and billing software. | Inconsistent data transfer leads to errors, denials, and delayed payments. | Implement integrated EHR and billing systems for smoother claim submission and faster payments. |
| Data-Driven Decision Making in AR Management | Ad hoc tracking and manual review of AR. | Lack of actionable insights into AR aging, slow resolution of bottlenecks. | Use data analytics to monitor AR trends, improve workflows, and predict payment cycles. |
Key AR Metrics Behavioral Health Practices Must Track in 2026
Tracking the right AR metrics is crucial for improving cash flow and reducing AR days. Below are the key metrics every behavioral health practice should monitor:
- Average AR Days: Keep AR days between 30-45. Anything over 60 days signals that there is inefficiency in the revenue cycle.
- AR Aging Breakdown: Segment AR by aging buckets: 0-30, 31-60, 61-90, 90+ days. Prioritize high-value claims and follow up on those sitting in the 61-90+ days category.
- Clean Claim Rate: Aim for 90%+ clean claims to reduce rework and ensure claims are processed without issues.
- Denial Rate by Payer: Track the denial rates by payer to identify patterns and take corrective actions with specific insurers.
- First-Pass Resolution Rate (FPRR): Maximize your first-pass resolution rate to ensure claims are paid without needing follow-up.
- Authorization-Related AR Percentage: Track how much AR is tied to missing or expired prior authorizations and act on it quickly.
- Patient Responsibility Collection Rate: With more patients moving to high-deductible health plans (HDHPs), managing patient balances upfront is essential.
Best Practices to Reduce AR Days in 2026
Reducing AR days in 2026 requires adopting best practices that streamline billing and improve collections. Here are the most effective strategies:
1. Clean Claim Submission
Ensure that all claims are submitted with accurate CPT/ICD-10 codes, modifiers, and complete documentation. The more accurate the claim, the less likely it is to be delayed or denied.
2. Telehealth Compliance Protocol
Standardize telehealth claims by applying the correct POS codes and modifier 95 for each payer. Ensure that your documentation clearly reflects the synchronous nature of the service to meet payer requirements.
3. Proactive Authorization Management
Track prior authorization expiration dates and submit renewals before the expiration period to ensure that claims aren’t delayed due to missing or expired authorizations.
4. Daily Denial Monitoring
Address denials within 24–48 hours to avoid aging claims. Quick action helps prevent delays in payments and reduces the time spent chasing payments.
5. Segment AR for Prioritization
Focus on high-dollar claims and those sitting in the 90+ days bucket. This helps prioritize resources and accelerates revenue recovery.
6. Monthly AR Review Meetings
Meet regularly with your billing team to review AR trends, payer patterns, and claim rejections. This ensures that you catch any issues early and resolve them efficiently.
7. Patient Responsibility Strategy
Collect co-pays and deductibles at the point of service. For high-deductible patients, offer payment plans and ensure that balances are paid faster.
How Cloud RCM Solution Helps Behavioral Health Practices in 2026
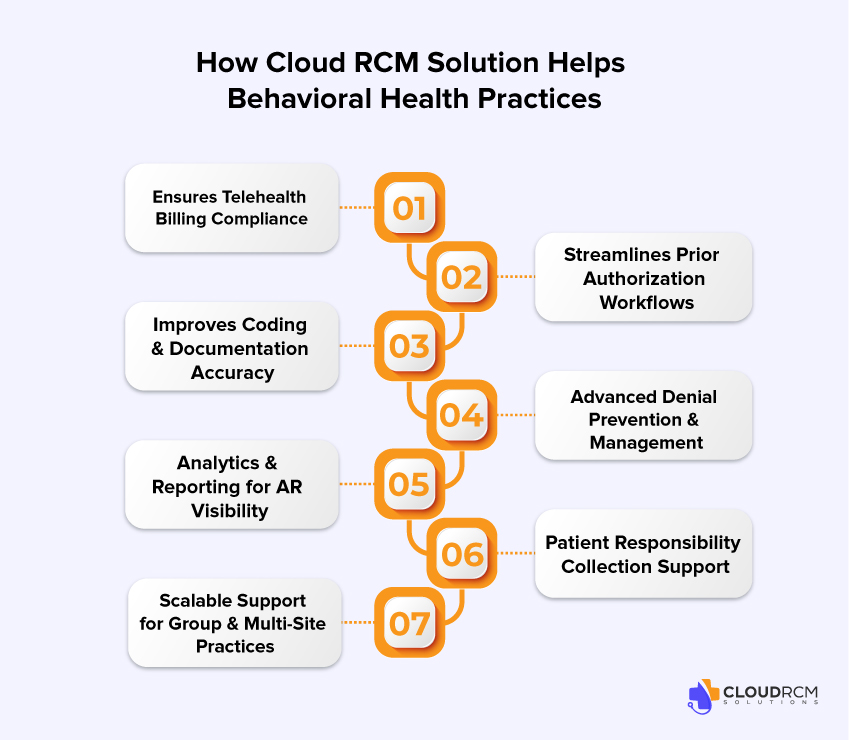
Cloud RCM Solution offers a comprehensive suite of tools to help behavioral health practices reduce AR days, streamline billing, and optimize cash flow:
1. Ensures Telehealth Billing Compliance
Our platform automatically applies the correct POS codes and modifier 95, and ensures your telehealth claims are compliant with payer-specific guidelines, minimizing denials and speeding up reimbursements.
2. Streamlines Prior Authorization Workflows
We track the status of every prior authorization in real-time, ensuring that all necessary authorizations are submitted on time and processed without delays.
3. Improves Coding & Documentation Accuracy
Our expert coding support ensures that your therapy and medication management claims are coded correctly. We provide guidance on how to properly document services to meet payer requirements and avoid rejections.
4. Advanced Denial Prevention & Management
We identify denied claims quickly, address the root causes, and resubmit them with the correct information. Our system helps prevent repeat denials, reducing AR aging and accelerating cash flow.
5. Analytics & Reporting for AR Visibility
Cloud RCM Solution offers real-time dashboards to track key AR metrics, including clean claim rates, denial trends, and payer performance, enabling better decision-making and strategic follow-ups.
6. Patient Responsibility Collection Support
We assist with upfront verification of patient balances, helping you collect co-pays and deductibles quickly. Our billing statements are optimized to ensure clarity and improve patient collections.
7. Scalable Support for Group & Multi-Site Practices
Whether you operate a single location or a multi-site practice, Cloud RCM Solution centralizes your AR management, ensuring consistent billing practices and faster collections across all sites.
Conclusion
In 2026, effectively managing AR days is critical to the financial stability of your behavioral health practice. With the complexities of telehealth billing, prior authorization delays, and inconsistent payer coverage, these challenges can severely impact your revenue cycle.
Don’t let AR days hold you back. By adopting best practices and leveraging Cloud RCM Solution, you can streamline your billing process, reduce AR days, and ensure quicker, more reliable reimbursements.
Let us handle the complexities of your billing and collections so you can focus on providing exceptional patient care and driving your practice’s growth.
Contact us today to learn how Cloud RCM Solution can transform your revenue cycle and secure your financial future.
What are Accounts Receivable (AR) days, and why are they important for behavioral health practices?
AR days measure the time between when a service is provided and when payment is received. Longer AR days slow cash flow, increase administrative costs, and impact your ability to invest in staff, technology, and growth.
Why are AR days increasing for behavioral health practices in 2026?
Telehealth billing complexity, frequent prior authorizations, inconsistent payer coverage, and documentation errors are the primary drivers of delayed payments, extending AR cycles to 60, 90, or even 120+ days.
How do telehealth billing errors affect AR days?
Incorrect POS codes, missing modifier 95, or payer-specific teletherapy rules can lead to claim denials or delays. Misapplied telehealth codes significantly increase AR aging and disrupt cash flow.
What role do prior authorizations play in AR delays?
Missing, expired, or incorrectly submitted prior authorizations can put claims on hold, preventing timely reimbursement. Efficient authorization tracking is crucial to keep AR days low.
How can documentation and coding errors increase AR?
Incomplete session notes, missing medical necessity justification, and inaccurate CPT/ICD-10 coding often trigger denials, requiring time-consuming appeals that prolong AR cycles.
Which AR metrics should behavioral health practices track in 2026?
Key metrics include Average AR Days, AR Aging Breakdown, Clean Claim Rate, Denial Rate by Payer, First-Pass Resolution Rate (FPRR), Authorization-Related AR Percentage, and Patient Responsibility Collection Rate.
How can Cloud RCM Solution help behavioral health practices reduce AR days?
Cloud RCM ensures telehealth compliance, automates authorization workflows, improves coding accuracy, prevents and manages denials, provides real-time AR analytics, and supports patient responsibility collection, all while reducing administrative burden.
Are telehealth claims more likely to be denied than in-person claims?
Yes. Telehealth claims are subject to payer-specific rules, modifiers, and POS codes. Without compliance, claims are more frequently denied or delayed compared to traditional in-person services.
How quickly should denials be addressed to minimize AR aging?
Denials should ideally be reviewed and corrected within 24–48 hours. Rapid rework prevents claims from re-entering AR aging cycles and accelerates revenue recovery.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine