Freestanding emergency rooms (FSERs) have become an increasingly important component of the healthcare landscape in Texas. Offering 24/7 access, faster treatment, and convenient locations outside of traditional hospitals, FSERs have rapidly grown to meet the demands of expanding urban and suburban populations. Cities like Dallas–Fort Worth, Houston, San Antonio, Austin, and El Paso now host over 200 licensed FSERs, making Texas the leading state in FSER proliferation.
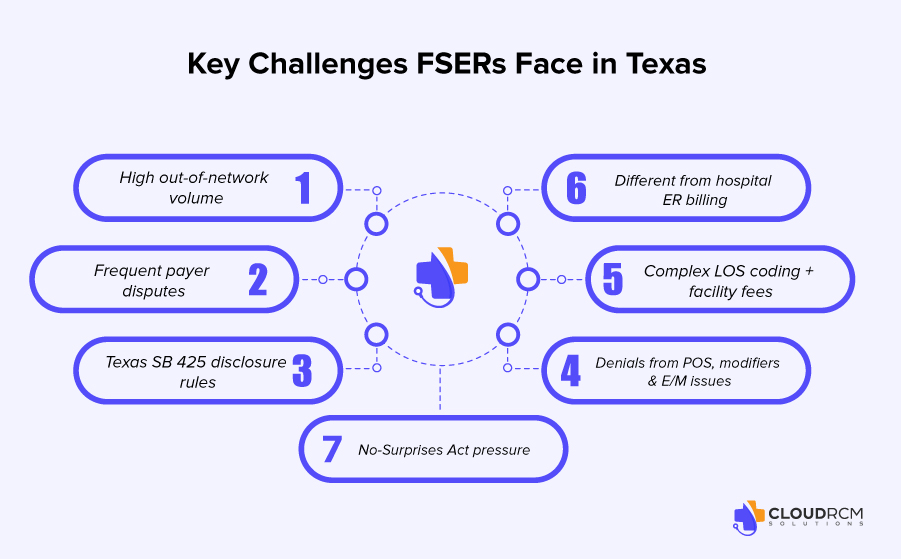
Despite their convenience and patient-focused advantages, FSERs face one of the most complex billing environments in the United States. Unlike hospital-based emergency rooms, FSERs operate under unique state regulations, federal legislation, and complex payer rules that can create revenue loss if not properly managed.
This article explores the landscape of Texas FSER billing, coding, compliance, common challenges, denials, and negotiation services, providing a clear picture of the current environment in 2025 and actionable insights for FSER operators.
The Rise of Freestanding Emergency Rooms in Texas
Over the past decade, FSERs have emerged as a solution to increasing demand for emergency services outside hospital settings. Several factors contribute to their growth:
- Population Expansion: Rapid urban and suburban growth has increased the demand for emergency care closer to residential areas.
- Convenience for Patients: FSERs provide shorter wait times and round-the-clock service, which is attractive for patients who prefer alternatives to crowded hospital ERs.
- Operational Flexibility: FSERs often have more flexible staffing and resource allocation, allowing them to manage patient flow efficiently.
However, this growth has also attracted heightened scrutiny from payers and regulators. Texas FSERs now contend with complex pricing transparency laws, mandatory disclosure requirements, federal No Surprises Act (NSA) rules, and stricter coding audits.
Why Texas FSER Billing Is Different from Hospital ER Billing
FSERs operate under unique conditions that make their billing more complex than hospital ERs or urgent care centers:
- State-Specific Regulations:
Texas mandates FSERs to clearly disclose information about facility fees, in-network vs. out-of-network status, and physician billing practices. Non-compliance can lead to fines, claim denials, and complaints. - Out-of-Network Prevalence:
Many FSERs function primarily as out-of-network facilities. While this allows flexibility in negotiations, it often results in payment delays and underpayments. - Complex Facility Fees:
Unlike urgent care centers, FSERs charge facility fees based on resources used, nursing intensity, and observation services. Proper coding is essential to ensure reimbursement accuracy. - Payer Scrutiny and Audits:
Insurers closely monitor FSER claims due to the higher likelihood of coding errors, duplicate charges, and misclassified services, which increases audit frequency and revenue risk.
Key Regulatory Updates for 2025
1. Texas Price Transparency Law
Texas law requires FSERs to:
- Post standard charges and facility fees prominently
- Notify patients about potential out-of-network billing
- Provide written consent for services when necessary
Failure to comply can lead to denials, fines, and patient complaints.
2. Mandatory Patient Disclosures
Under Texas Health & Safety Code §254, FSERs must disclose:
- Network status of the facility
- Expected out-of-pocket costs
- Separate billing by physicians or ancillary services
Non-compliance is one of the top reasons FSERs face complaints to the Texas Attorney General.
3. No Surprises Act (NSA) Compliance
The federal NSA protects patients from surprise bills and requires:
- Good-faith cost estimates
- Dispute resolution mechanisms for out-of-network claims
- Compliance with federal timelines and calculation requirements
Texas FSERs experience the highest out-of-network dispute rates in the U.S., particularly in specialties like emergency medicine, radiology, cardiology, trauma care, and behavioral health evaluations.
Common Billing and Coding Challenges for FSERs
1. Evaluation & Management (E/M) Coding
FSERs use CPT codes 99281–99285 to bill for patient visits. Proper E/M coding depends on:
- Patient complexity
- Medical decision-making (MDM)
- Length of stay (LOS)
- Resources utilized
A 2024 Texas audit revealed that 43% of ER visits were downcoded due to insufficient documentation or unclear MDM.
2. Facility Fee Coding
Facility fees are central to FSER reimbursement. Accurate coding must reflect:
- Resource consumption
- Nursing intensity
- Observation services
- Procedural interventions
Errors can lead to underpayment, recoupments, or delayed revenue.
3. Ancillary and Procedure Coding
- Radiology, laboratory, and procedural services must be coded correctly.
- Injection/infusion hierarchies and point-of-care testing require attention to detail.
Improper coding increases denial rates and audit exposure.
Top Denial Reasons for Texas FSERs
FSERs face denials for multiple reasons, including:
- Out-of-Network Payment Disputes
- Medical Necessity Denials
- Coding Errors and Modifier Misuse
- Incorrect Place of Service (POS) Codes
- Insufficient E/M Documentation
- Authorization Conflicts for Ancillary Services
- Missing or Incorrect Patient Disclosures
Specialties most affected include emergency medicine, radiology, orthopedics, cardiology, and behavioral health.
Best Practices for FSER Revenue Cycle Management
1. Real-Time Eligibility Verification
Ensures claims are submitted correctly and reduces coordination-of-benefits errors.
2. Documentation Alignment
Coders and clinicians must ensure documentation supports billed E/M levels, procedures, and observation services.
3. Denial Prevention & Management
CloudRCM identifies recurring claim issues to prevent rejections before submission. Patterns such as modifier errors, missing documentation, or POS misalignment are addressed proactively.
4. Out-of-Network Reimbursement Monitoring
Texas FSERs often receive 10–40% less than expected without monitoring. CloudRCM tracks OON payments, identifies discrepancies, and manages appeals.
5. Payer Contract Negotiation
CloudRCM negotiates contracts to:
- Improve reimbursement rates
- Ensure compliance with NSA and Texas law
- Guide Independent Dispute Resolution (IDR)
CloudRCM FSER Services
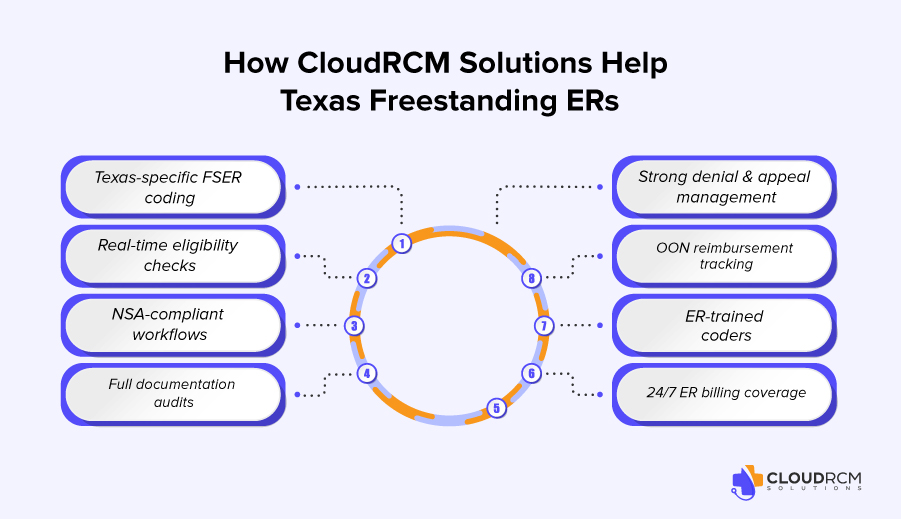
CloudRCM provides full-cycle FSER billing, coding, compliance, and negotiation services:
- Texas-specific coding and facility fee management
- Real-time insurance verification and eligibility checks
- Full NSA compliance workflows
- Denial and appeal management
- Out-of-network reimbursement monitoring
- ER-trained coding teams
- 24/7 operational billing workflows
- Strategic payer negotiation
Outcome Benefits: Reduced denials, faster collections, stronger cash flow, and improved OON reimbursements.
Patient Financial Communication and Transparency
Effective patient communication reduces disputes and supports compliance:
- Transparent facility fee disclosures
- Cost estimates per NSA requirements
- Written consent for OON services
- Staff training on patient financial discussions
This proactive approach improves patient satisfaction and decreases claim denials.
Data Analytics and Technology in FSER RCM
CloudRCM leverages analytics to:
- Predict denial risks
- Monitor payer trends
- Optimize coding and documentation
- Support OON negotiations and dispute resolution
This technology-driven approach ensures higher reimbursement and compliance while reducing administrative burden.
Competitive Advantages of CloudRCM
Unlike many competitors, CloudRCM emphasizes:
- Texas-specific FSER regulatory expertise
- Strategic OON payer negotiation
- Patient transparency and financial education
- Data-driven analytics for denial prevention
- Audit-ready documentation and compliance support
These advantages ensure FSERs maximize revenue while maintaining regulatory compliance.
FSER Coverage Areas
CloudRCM supports FSERs across Texas:
- Dallas–Fort Worth
- Houston
- San Antonio
- Austin
- El Paso
We also provide services in Oklahoma, Arizona, Florida, and Colorado.
Conclusion
Billing and managing freestanding ERs in Texas is complex and highly regulated, making proper revenue cycle management critical. Between high denial rates, regulatory updates, complex coding, and payer disputes, FSERs risk significant revenue loss without expert guidance.
CloudRCM Solutions provides end-to-end FSER billing, coding, compliance, and negotiation services, combining Texas-specific expertise, data-driven insights, and payer negotiation strategies to help FSERs maximize revenue, reduce denials, and maintain compliance in 2025 and beyond
FAQs
How is FSER billing different from hospital ER billing?
FSERs must comply with Texas price transparency laws, disclosures, and frequently operate OON, which hospital ERs rarely experience.
How can FSERs reduce denials in 2025?
Align documentation, verify patient eligibility, code accurately, monitor OON reimbursements, and comply with Texas laws.
What are CloudRCM’s negotiation services?
We provide strategic payer contract evaluation, benchmark analysis, OON negotiation workflows, and support IDR processes.
How does CloudRCM help with compliance?
By monitoring regulatory changes, auditing documentation, ensuring price transparency, and implementing NSA-compliant workflows.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine