Feeling overwhelmed by the administrative demands of Fertility billing and coding? You’re not alone. With IVF cycles costing between $12,000 and $30,000, and total expenses potentially exceeding $61,000 to achieve a live birth, accurate billing is crucial to prevent financial strain on both patients and providers.
Moreover, only about 25% of U.S. employers offer insurance coverage for IVF treatments, leaving many patients to shoulder these substantial costs themselves.
What Are IVF Billing Services and Why Are They Important?
IVF stands for In Vitro Fertilization, a medical procedure used to help individuals and couples with infertility achieve pregnancy. In the healthcare industry, IVF billing involves documenting and coding infertility treatments for insurance claims and financial records.
This process ensures timely reimbursement for healthcare providers and minimizes patients’ out-of-pocket expenses. Reproductive medicine billing encompasses various procedures, from consultations and diagnostics to advanced treatments like sperm aspiration and embryo transfers.
Improving Patient Communication in Fertility Billing
Effective medical billing and insurance coverage communication is essential to reduce patient stress during their fertility journey. Providers should:
- Offer detailed cost breakdowns, including estimated out-of-pocket expenses.
- Use patient-friendly language to explain insurance benefits and limitations.
- Assign dedicated financial counsellors to guide patients through billing, ensuring clarity and trust.
CPT Codes for IVF Billing
CPT codes (Current Procedural Terminology) are essential for documenting specific IVF-related procedures. Below is a table summarizing key CPT codes used in reproductive medicine billing:
| CPT Code | Description | Usage |
| 58970 | Follicle puncture for oocyte retrieval | Used for oocyte (egg) retrieval in IVF cycles |
| 58974 | Embryo transfer | Covers the procedure of embryo implantation |
| 58322 | Artificial insemination | Used for intrauterine insemination (IUI) |
| 89261 | Sperm isolation (complex prep) | For procedures like gradient preparation |
| 89320 | Sperm evaluation, complete | Comprehensive sperm analysis |
| 89342 | Storage of sperm | Used for cryopreservation of sperm samples |
Modifiers in IVF Billing
Modifiers provide additional details about the procedure used in the IVF treatment, helping insurers process claims accurately. Examples include:
- Modifier 26: Professional component (e.g., physician’s interpretation of lab results).
- Modifier TC: Technical component (e.g., use of lab equipment).
- Modifier 59: Distinct procedural service, indicating that a procedure is separate from others performed on the same day.
Improving Technology for Efficient IVF Billing
Advanced tools and software can simplify Fertility billing and reduce errors. Practices can adopt:
- Electronic Health Records (EHR): Integrate billing and coding directly with patient records for accuracy.
Common Mistakes in IVF Billing and How to Avoid Them
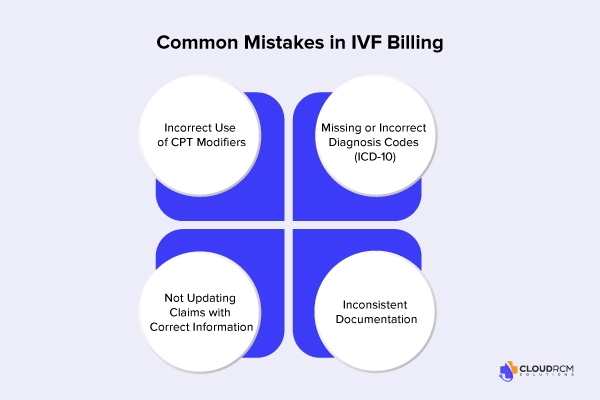
Efficient medical billing and coding are crucial for a successful IVF reimbursement, but mistakes are common. Here are some frequent billing errors and tips on how to avoid them:
1. Incorrect Use of CPT Modifiers:
Misusing or using wrong modifiers can lead to claim rejections or delays. For example, using Modifier 59 incorrectly to indicate separate procedures on the same day can cause issues with insurers. Providers should ensure they understand when and how to use each modifier, such as Modifier 26 for professional services or Modifier TC for technical services.
2. Missing or Incorrect Diagnosis Codes (ICD-10):
Failing to match the correct ICD-10 diagnosis code to the IVF procedure can lead to claim denials. Ensure that the diagnosis justifies the treatment provided, such as coding for male infertility or fallopian tube issues.
3. Not Updating Claims with Correct Information:
IVF cycles often involve multiple steps, including oocyte retrieval, embryo transfer, and medication administration. Each step must be properly coded and billed. Missing or outdated codes can cause delays in reimbursement.
4. Inconsistent Documentation:
Incomplete or vague documentation can lead to a lack of clarity in coding. Ensure all treatment stages, from initial consultation to follow-up care, are well-documented.
How To Deal With Denied IVF Claims?
Denied claims can disrupt both the providers and patients. To address denials:
- Identify the Cause: Review the denial code or reason provided by the insurer.
- Gather Documentation: Collect relevant medical records and proof of procedure necessity.
- Submit an Appeal: Draft a detailed letter with supporting documents, citing specific insurer policies.
- Follow-up: Monitor the claim status and maintain communication with the payer.
What is the Importance of Coding Verification?
Coding verification is crucial to ensure accuracy and avoid claim denials. Errors in coding are among the most common reasons for reimbursement delays in reproductive medicine billing. A study published in the Journal of Healthcare Management found that incorrect coding can lead to a denial rate of up to 20%. Another study found that using modifiers can increase reimbursement rates by up to 10%. Comprehensive verification involves:
- Confirming the appropriateness of ICD-10 and CPT codes.
- Ensuring consistency with medical documentation.
- Validating modifiers to provide context for services.
Insurance Verification for IVF
Insurance verification for infertility treatment or IVF is very crucial. This step ensures that patients who are struggling with infertility receive the treatments they need without unexpected financial surprises. Beyond eligibility and benefits, the process includes:
- Confirming the IVF procedure and associated services are covered under the patient’s policy.
- Identifying any exclusions or restrictions related to infertility treatments, such as waiting periods or specific medical conditions.
- Assess whether the patient’s insurance requires referrals or additional documentation for IVF services.
- Determining the network status of the fertility clinic to avoid out-of-network costs.
- Providing a detailed breakdown of what the insurance covers and what the patient will need to pay out-of-pocket, including co-pays, co-insurance, and deductibles.
Common Insurance Challenges in IVF
IVF treatment presents specific insurance challenges. Understanding these challenges can help providers navigate the complexities of billing and reimbursement.
- Pre-Authorization Requirements:
Many insurance companies require pre-authorization for IVF services. Claims can be denied without prior approval, which can delay treatment and reimbursement. Providers should have a system in place to handle these approvals efficiently.
- Denied Claims for Non-Covered Services:
IVF treatments are not always fully covered, and insurers may deny claims for certain procedures like egg freezing, embryo freezing, or genetic testing. If this happens, providers should ensure they know the proper steps for appealing these denials, including submitting additional documentation or requesting a review.
- Insurance Plan Limitations:
Some policies place limits on the number of IVF cycles covered per year or lifetime. Providers should be aware of these limits to inform patients beforehand and avoid surprises.
Does Insurance Cover All IVF Services?
While some insurance plans cover diagnostic testing and medications, others may exclude advanced procedures like IVF or limit coverage to specific diagnoses. Patients should inquire about: Most insurance plans cover diagnostic testing and medication.
- Coverage for donor sperm or egg services.
- Requirements for undergoing fewer treatments, such as IUI, before IVF.
- Conditions that could result in denial such as prior failed cycles or sterilization.
State-Specific Regulations and Reimbursement Policies
There are some state-specific regulations and reimbursement policies:
State Mandates:
Some states, like California and Massachusetts, require insurers to cover IVF under specific conditions. Providers must stay informed about these mandates to ensure compliance.
Out-of-State Care:
When patients seek treatment outside their home state, providers should verify whether their insurance plan covers IVF in other states and check for any network limitations.
Customizing Billing for State-Specific Plans:
Billing requirements vary by state, particularly in states with IVF mandates. Providers should be aware of pre-certification or documentation requirements that may affect claim approval and reimbursement timelines.
The Human Connection in Fertility Billing
Beyond numbers and codes, Fertility billing is about enabling patients to achieve their dreams of parenthood. Clear communication about costs and coverage helps build trust and reduce stress during this emotional journey.
Importance of Staff Training in IVF Billing
Proper staff training ensures the efficient use of IVF coding, modifiers, and insurance requirements. Regular workshops, certifications, and updates on coding guidelines (e.g., CPT and ICD-10) are vital for maintaining accuracy and compliance.
Final Thought:
The Fertility billing services require expertise, attention to detail, and a patient-centric approach. By understanding the complexities of coding, insurance verification, and financial planning, providers can deliver exceptional care to patients while optimizing reimbursement. Whether you’re a patient exploring IVF options or a provider refining your billing processes, staying informed is the key to success in reproductive medicine billing.
For more insights and personalized assistance, reach out to CloudRCM Solutions at (224) 231-6880 or schedule a free meeting with our team to discuss how we can simplify your IVF billing process and maximize reimbursements.
FAQs:
Is IVF usually covered by insurance?
It depends on the patient’s plan and state laws—some cover it fully, others don’t at all.
What are the common CPT codes used for IVF?
Common codes include 58970 (follicle aspiration), 89250–89268 (lab handling), and others for ultrasounds and consultations.
How do I bill for embryo transfer?
Use CPT code 58974 for fresh embryo transfer and 58976 for frozen.
Should I use modifiers when billing IVF services?
Yes, modifiers like -TC or -26 may be needed based on service location and who performed it.
Can patients use HSAs or FSAs for IVF expenses?
Yes, in most cases, IVF-related costs can be paid using HSA or FSA funds.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine


