You care for families, who’s caring for your cash flow? Family medicine is fast-paced and diverse. One hour it’s a child’s vaccine, the next it’s managing a chronic illness. But with that variety comes billing complexity, and that’s where many practices lose money.
Did you know 1 in 4 family medicine claims gets denied or delayed due to coding or documentation errors? That’s lost revenue you can’t afford to ignore.
Family medicine billing services help you get paid faster, with fewer headaches, so you can focus on care, not claims.
What Is Medical Billing In Family Medicine?
Medical billing in family medicine involves converting patient visits into standardized codes to submit claims for insurance reimbursement. Since family doctors treat all ages and a wide range of conditions, billing must cover everything from routine checkups to chronic care, making accuracy and compliance essential for timely payments.
Common challenges in family medicine medical billing
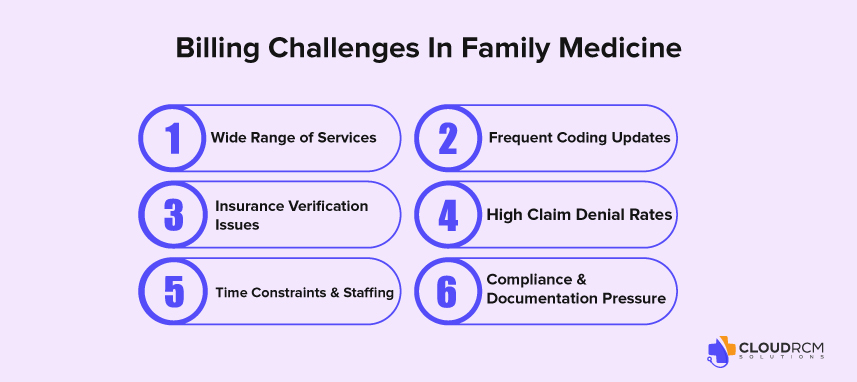
Medical billing for family practice isn’t as simple as it seems. While the care is holistic, the billing is anything but, because family physicians treat a wide range of conditions across all age groups. That means billing teams must stay updated, organized, and quick to adapt. Here are some of the top challenges:
Wide Range of Services
From infant wellness visits to geriatric chronic care, family practices handle it all, each requiring different codes, modifiers, and documentation. That variety increases the chances of billing errors.
Frequent Coding Updates
ICD-10 and CPT codes are updated regularly. Missing even a small change can lead to denials or underpayments.
Insurance Verification Issues
With patients switching plans or providers frequently, verifying coverage for each visit is time-consuming, but essential to avoid claim rejections.
High Claim Denial Rates
Small errors in patient info, codes, or documentation can lead to delays or denials. And family practices usually see a high volume of claims, compounding the problem.
Time Constraints & Staffing
Front-desk staff often juggle billing with other tasks, increasing the risk of mistakes. Practices without a dedicated billing team struggle to keep up.
Compliance & Documentation Pressure
Detailed documentation is crucial not just for billing, but for audits. Family practices must ensure clinical notes align with what’s billed to avoid penalties.
The Hidden Cost of Billing Errors in Family Medicine
Denied or underpaid claims aren’t just paperwork problems; they’re silent revenue killers. On average, family medicine practices lose $30,000 to $100,000 per year due to coding errors, missed modifiers, or incomplete documentation. With tight margins and high patient volume, even a small increase in billing accuracy can significantly boost your revenue cycle performance.
Best Practices for Family Practice Medical Billing
Billing keeps your practice alive; get it wrong, and revenue slips fast. From wellness visits to chronic care, every patient encounter must be coded and submitted just right. These quick tips will help keep your claims clean and cash flow steady:
Double-Check Patient & Insurance Info
Always verify patient details and insurance coverage at every visit. Even a small error in name spelling or policy number can lead to claim rejections.
Keep Documentation Tight & Aligned
Ensure your clinical notes support the services you bill for. Incomplete or vague documentation is one of the top reasons for denials and audit issues.
Stay Updated on Coding Changes
ICD-10 and CPT codes change often, especially with new guidelines for E/M services. Regular updates and training help you avoid costly coding mistakes.
Submit Claims Quickly and Cleanly
The faster and cleaner your claim, the quicker you get paid. Aim to submit claims within 48–72 hours of the visit and use claim scrubbing tools to reduce errors.
Follow Up on Denials Proactively
Denied claims are not the end, just the beginning. Have a system in place to track, correct, and resubmit them without delay.
Make Patient Billing Clear
Avoid confusion and billing delays by clearly explaining patient responsibilities. Collect copays upfront and send easy-to-read statements.
Train Your Team Regularly
Billing and coding rules evolve fast. Keep your staff in the loop with short training sessions and quick coding refreshers every few months.
Run Internal Billing Audits
Routine checks help catch small errors before they become big problems. Audit claims, coding accuracy, and payment patterns regularly.
Common CPT codes used in family medicine medical billing
| CPT Code | Description | Use Case |
| 99201–99205 | New patient office visits (levels 1–5) | First-time patient appointments |
| 99211–99215 | Established patient office visits (levels 1–5) | Follow-up or routine checkups |
| 99381–99387 | Preventive visits (new patients, age-based) | Annual wellness for new patients |
| 99391–99397 | Preventive visits (established patients, age-based) | Routine physicals for existing patients |
| 99406–99407 | Smoking cessation counseling | Tobacco use counseling |
| 99495–99496 | Transitional care management | Follow-up after hospital discharge |
| 99401–99404 | Preventive counseling (individual, 15–60 mins) | Lifestyle, diet, mental health guidance |
| 99408–99409 | Alcohol and substance abuse screening/intervention | Brief intervention for substance use |
| 96127 | Brief emotional/behavioral assessment | Depression or anxiety screening |
| 36415 | Routine venipuncture | Blood sample collection |
| 81002–81003 | Urinalysis (non-automated/automated) | Basic diagnostic testing |
| 90658 | Influenza vaccine administration | Seasonal flu shot |
In-House vs. Outsourced Billing:
As family medicine practices face increasing administrative burdens, choosing between in-house billing and outsourcing has become a strategic decision that directly affects revenue cycle performance and practice efficiency.
In-House Medical Billing
While some practices prefer to keep billing internal for control, it often comes with challenges:
- Resource-Intensive – Requires dedicated staff, ongoing training, and regular compliance updates.
- Limited Expertise – General billing staff may not specialize in family practice-specific coding and payer nuances.
- Slower Denial Management – Limited bandwidth can delay follow-ups, impacting collections and cash flow.
Outsourced Billing Services
Outsourcing to a specialized partner offers measurable advantages:
- Expertise in Family Medicine Billing: Trained teams handle complex coding, modifiers, and payer-specific rules.
- Cost-Effective: Reduces overhead costs related to software, staffing, and training.
- Improved Efficiency: Faster claim submissions, lower denial rates, and better revenue tracking.
- Scalable Support: Grows with your practice and adapts to changing billing regulations.
Telehealth Billing in Family Medicine:
With the rise of virtual care, telehealth billing has become essential for family medicine practices. To ensure full reimbursement, providers must use Modifier 95 when billing eligible telehealth services and follow payer-specific guidelines. Incorrect coding or missing modifiers can lead to unnecessary denials and revenue loss.
Final Thoughts:
Family medicine is about providing lifelong care from first checkups to chronic disease management. But billing for such diverse services requires more than just coding knowledge; it demands consistency, compliance, and strategic oversight. When even minor billing errors can cost thousands annually, getting it right is not optional; it’s essential.
By improving your billing operations, staying ahead of coding changes, and following best practices, your family practice can transform billing from a burden into a reliable source of revenue growth.
Ready to Simplify Family Medicine Billing?
At CloudRCM, we specialize in helping family medicine practices reduce claim denials, improve reimbursement accuracy, and regain valuable time. Whether you’re struggling with high denial rates, outdated billing workflows, or telehealth complexities, our expert team delivers end-to-end support tailored to your needs.
Schedule a free consultation now and get a customized strategy for improving your family medicine revenue cycle.
FAQs:
What is Family Medicine Medical Billing?
It’s the process of converting family care services like check-ups and chronic care into codes for insurance reimbursement.
How is Family Medicine Billing Different from Other Specialties?
It covers all age groups and conditions, requiring broader coding and insurance knowledge.
What are the Key Components of Family Medicine Medical Billing?
Patient intake, insurance checks, accurate coding (CPT, ICD-10), claim submission, and EOB management.
What are the Common Challenges in Family Medicine Billing?
Frequent coding updates, diverse services, insurance rules, and patient billing communication.
How Can Family Practices Optimize Their Billing?
Use smart workflows, EHR-integrated billing, accurate documentation, ongoing training, and proactive denial follow-ups.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine