In healthcare, Chiropractic credentialing is the process by which a chiropractor gets affiliated or makes agreements with insurance companies so they can accept reimbursements for the visits of patients. This helps grow the patient base for the services you are providing.
Are you a chiropractor and you want to be credentialed? In the ever-evolving healthcare industry, Chiropractors often face unique challenges when building a healthy practice. Among these, Chiropractic Credentialing proves to be a critical step for securing a stable patient base and ensuring the financial stability of the practice. While it may seem like a very difficult administrative task, the benefit it offers is more transformative. When you are aligned with insurance companies, it opens the door to a larger pool of patients, boosts your credibility and improves your practice.
Why Do Patients Value Chiropractors Who Are Credentialed?
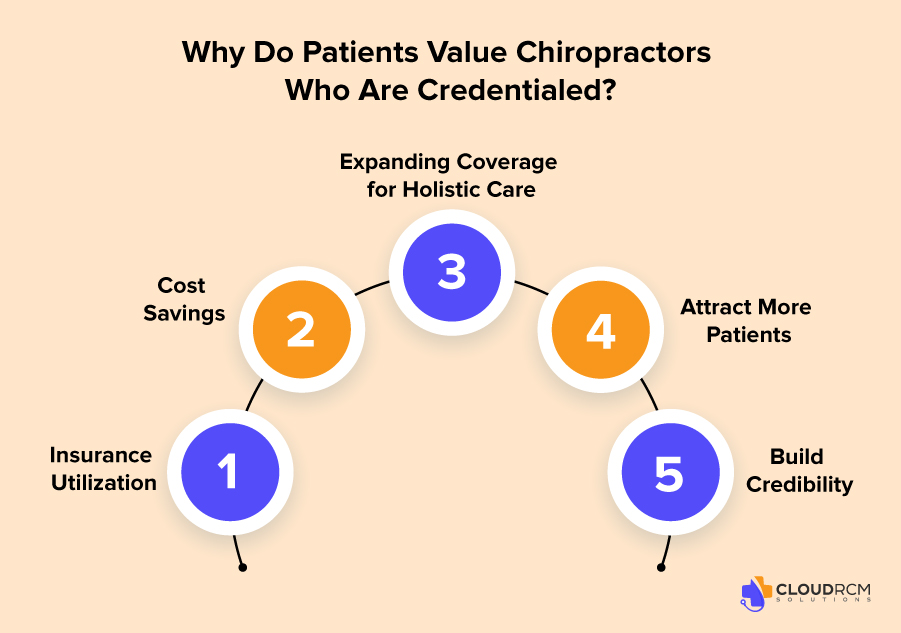
Credentialed Chiropractors are more trusted and visited by patients; it becomes more convenient and affordable for the patients when seeking healthcare. Here’s why credentialing matters to them:
- Insurance Utilization: A survey by HealthMarkets revealed that 63% of patients choose providers based on whether their insurance is accepted. Without credentialing, you risk losing potential clients to competitors.
- Cost Savings: It is more convenient and affordable for patients. In-network providers reduce out-of-pocket expenses, making services more accessible.
- Expanding Coverage for Holistic Care: Modern insurance plans increasingly cover chiropractic care, acupuncture, and physical therapy, reflecting a growing demand for integrative healthcare solutions.
- Attract More Patients: According to a 2022 healthcare report, nearly 78% of Americans rely on insurance for their healthcare needs, making credentialing vital to appeal to insured patients.
- Build Credibility: Being “in-network” with major insurance companies signals professionalism and adherence to industry standards, fostering trust.
What Are The Steps to Improve Chiropractic Credentialing Successfully?
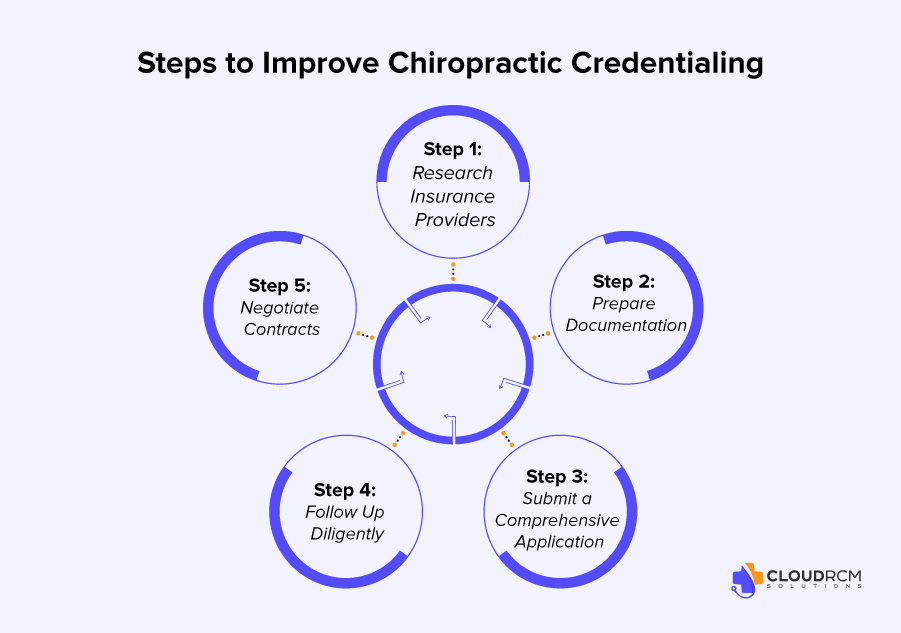
The Credentialing process might seem difficult, but when you have clear plans, you can simplify the whole process for your service.
Here’s a step-by-step approach:
Step 1: Research Insurance Providers
Before you get credentialed with any insurance company, you need to do some research to see if that will work for you. Evaluate which insurance networks align with your practice goals. Factors to consider include:
- Reimbursement Rates: Are they competitive?
- Patient Base: Does the provider cater to your target demographic?
- Requirements: What documentation and qualifications are needed?
Step 2: Prepare Documentation
To get credentialed, you need to provide appropriate or accurate documentation. Any misinformation in the documentation can lead to delays and rejection. Ensure you have the following on hand:
- State license and national certifications.
- Proof of malpractice insurance.
- National Provider Identifier (NPI) number.
- Educational credentials
- Training records.
- licensure
Step 3: Submit a Comprehensive Application
If you want the process of credentialing to be quicker and accurately. Many applications are now digital you can use them to avoid delays:
- Double-check for errors or missing details.
- Include all required documents.
- Provide accurate billing and contact information.
Step 4: Follow Up Diligently
The credentialing process can take anywhere from 90 days to six months. Regularly check the status of your application and quickly address requests for additional information.
Step 5: Negotiate Contracts
Don’t hesitate to negotiate reimbursement rates to ensure they align with the value you are providing.
Chiropractic Credentialing Checklist:
- Verify educational qualifications
- Confirm active state licensure
- Ensure valid malpractice insurance
- Collect work history and experience
- Check continuing education requirements
- Conduct a background check (if required)
- Verify identity and legal eligibility
- Complete and submit the credentialing application
- Apply for insurance network enrollment
- Review credentialing policies and procedures
- Provide professional references (if required)
- Track re-credentialing timelines
How Credentialing Benefits Chiropractic Practices?
Credentialing goes beyond paperwork, it’s a strategic move to grow your practice.
- Broaden Your Reach: Insurance affiliation connects you to a wider audience.
- Enhance Patient Retention: In-network patients are more likely to return.
- Diversify Revenue: Expand into services like massage therapy and physical rehabilitation.
| Benefit | Impact |
| Increased Patient Base | Access to insured patients, boosting appointments by up to 40%. |
| Improved Credibility | Establishes trust and professionalism with patients and peers. |
| Higher Revenue Potential | Enables claims for a variety of covered treatments. |
| Competitive Advantage | Differentiates you from cash-only practices. |
Common Challenges and How to Overcome Them
- Lengthy Process: Credentialing can be time-consuming. But you can solve the issue as well by starting early and considering professional help.
- Rejections: Applications may be denied due to incomplete information. Therefore, you need to double-check documents and provide thorough details.
- Administrative Burden: Managing multiple insurance contracts can be overwhelming, but when you are using specialized software or delegating tasks to trained staff, that can prove to be very helpful.
How to Maximize the Impact of Being Credentialed?
Credentialing is only the first step. To reap its full benefits:
Market Your In-Network Status:
- Highlight accepted insurance plans on your website, social media, and marketing materials.
- Train front-desk staff to inform patients about insurance coverage.
Stay Updated on Policies:
- Attend webinars and industry events to stay informed about changing insurance guidelines.
- Periodically review contracts to ensure favourable terms.
Outsource to medical billing services:
- You can outsource efficient and reliable medical billing & coding to decrease the administrative burden.
- Choose the right medical billing firm that shows compliance with the regulatory policies.
Final Thought:
Chiropractic Credentialing is crucial it is a strategic tool that can redefine your practice’s growth. Patients find it more convenient and affordable and getting credentials helps Chiropractors to improve the patient base because the service is now more accessible to insured patients. Gaining the trust of patients is very important for every healthcare provider. By doing so, you position yourself as a trusted and credible provider in the healthcare community.
The process may require effort, but the rewards from increased patient volume to enhanced financial stability make it worthwhile. For chiropractors ready to grow their practice, now is the time to embrace credentialing as a cornerstone of success.
Transforming Your Practice with CloudRCM
Handling the credentialing is an additional administrative task that can be very overwhelming for your staff. We have good news for you, we can help you by doing credentialing. While you can focus on your goal of providing exceptional care to the patient. CloudRCM has a dedicated team that shows compliance with the evolving regulations and policies.
We want to solve your issues related to credentialing. Schedule an appointment today or contact us at (224) 231-6880.
FAQ’s
What are the most common reasons for credentialing delays or denials?
Delays often occur due to missing paperwork, inaccurate details, or slow payer responses. Applications are sometimes denied for incomplete CAQH profiles, outdated licenses, or missing malpractice coverage. Always double-check documents and maintain accurate provider data.
How often do chiropractors need to recredential?
Most insurance companies require recredentialing every 2–3 years to ensure your credentials and compliance remain current. This process updates your licensure, malpractice coverage, and certifications to maintain network participation.
How does credentialing benefit chiropractic practices financially?
Credentialing connects your practice with insured patients, which can increase patient volume by up to 40%. It improves cash flow through consistent reimbursements, enhances patient retention, and strengthens your professional credibility with both patients and insurers.
Does CloudRCM offer chiropractic billing services too?
Yes, CloudRCM provides end-to-end medical billing and credentialing services for chiropractors. Our solutions reduce claim denials, improve cash flow, and ensure compliance with payer policies — helping your practice grow sustainably.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine