In 2026, cardiology practices are facing a critical challenge: rising reimbursement delays, skyrocketing denial rates, and increasing patient financial responsibility are draining cash flow and leaving revenue unpaid. With so much earned revenue left on the table, ineffective AR management is directly impacting your practice’s financial stability. To thrive, it’s no longer enough to just submit claims; you need a comprehensive strategy that tackles payer issues, reduces denials, and ensures fast, accurate payments. Whether you’re a solo cardiologist or a large multi-location group, mastering AR management is essential to protect your practice’s bottom line.
Why AR Management for Cardiology Practices Is More Challenging in 2026
Cardiology billing is inherently complex, which makes cardiology AR management far more demanding than many other specialties. Cardiac procedures often involve multiple CPT codes, modifiers, and bundled services that must meet strict payer guidelines. Even small discrepancies in coding or documentation can result in claim denials or delayed reimbursements.
In 2026, payer scrutiny has intensified, especially among Medicare and Medicare Advantage plans. Industry data shows that while the average medical claim denial rate ranges between 10–15%, cardiology practices frequently experience denial rates closer to 18%. These denials significantly impact accounts receivable management in cardiology by increasing AR aging and staff workload.
Additionally, cardiology practices in states such as California, Texas, Florida, and New York face varying payer rules and authorization requirements, making cardiology billing and AR services more challenging to standardize across locations.
The Financial Impact of Poor Cardiology AR Management
Inefficient cardiology AR management does more than delay reimbursement; it disrupts the entire revenue cycle. When AR management for cardiology practices is not closely monitored, claims move slowly through follow-up cycles and often age into the 90+ day bucket, where recovery rates drop dramatically.
According to industry benchmarks, days in AR cardiology benchmarks suggest that high-performing practices keep AR below 40 days. However, many cardiology clinics continue to operate at 45–55 days or more. This extended AR cycle limits cash flow, increases write-offs, and makes it harder to invest in staffing, technology, and patient care.
For cardiology practices in high-volume markets like Florida and Pennsylvania, even a small increase in AR days can translate into hundreds of thousands of dollars tied up in unpaid claims.
Key AR Metrics Every Cardiology Practice Should Track
Days in Accounts Receivable
Days in AR is one of the most important indicators of cardiology AR management performance. Monitoring days in AR cardiology benchmarks helps practices identify delays in follow-up and payer processing. Practices that consistently exceed benchmark ranges often struggle with inefficient workflows or limited AR resources.
Net Collection Rate
A strong net collection rate reflects effective accounts receivable management in cardiology. Cardiology practices should aim for a net collection rate of 95% or higher. Lower rates often indicate missed follow-ups, underpayments, or unresolved denials.
Aging AR Buckets
Breaking down AR into 0–30, 31–60, 61–90, and 90+ day buckets allows practices to prioritize follow-up efforts. Effective AR follow-up for cardiology focuses on resolving claims before they reach the 90-day mark, where recovery becomes more difficult.
Common AR Challenges in Cardiology Practices
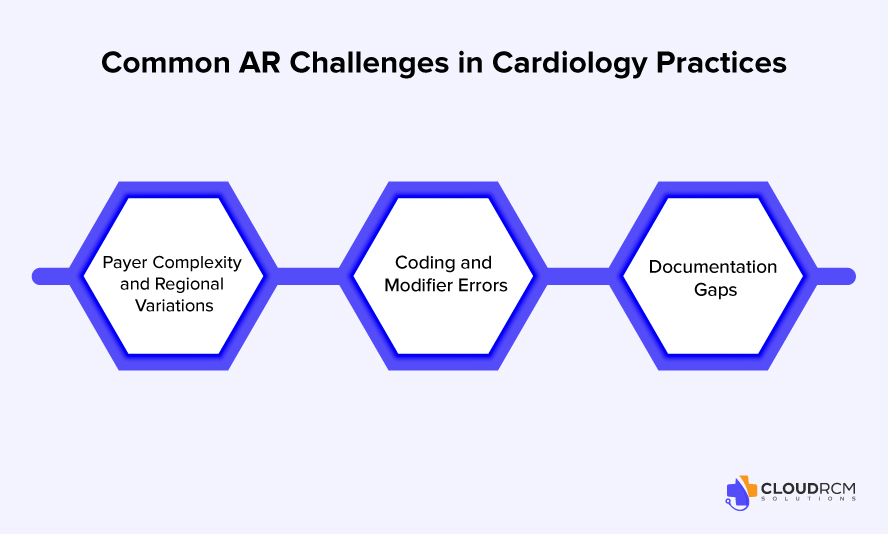
Payer Complexity and Regional Variations
Cardiology practices work with a wide range of payers, each with unique rules and reimbursement policies. Medicare cardiology AR challenges are particularly common due to strict medical necessity requirements and frequent policy updates. In states like Texas and Arizona, Medicare Advantage plans account for a large share of cardiology AR, increasing denial risk.
Coding and Modifier Errors
Accurate coding is essential to cardiology billing and AR services. Modifier misuse, especially for -25, -26, -TC, and -59, remains a top contributor to cardiology claims denial trends. Even experienced billing teams must stay current with payer-specific coding updates to prevent avoidable denials.
Documentation Gaps
Incomplete or unclear documentation directly affects accounts receivable management in cardiology. Missing diagnostic reports or insufficient clinical justification can result in medical necessity denials, increasing AR aging and appeal volume.
Patient Financial Responsibility and Its Role in Cardiology AR
Patient responsibility continues to rise in 2026, reshaping cardiology AR management strategies. High-deductible health plans mean patients are responsible for a larger portion of cardiac care costs, particularly for advanced imaging and procedures.
When eligibility verification and benefit explanations are not handled upfront, balances shift into patient AR, which is harder to collect than insurance AR. Practices that want to improve cash flow for cardiology clinics must focus on clear communication, upfront estimates, and timely patient billing to prevent balances from aging.
Denial Management as a Core Component of AR Management for Cardiology Practices
Denial management is one of the most critical drivers of financial performance in cardiology AR management. Because cardiology services involve high-dollar procedures and complex payer rules, even small denial trends can significantly increase AR aging if not addressed systematically.
Eligibility and Coverage-Related Denials
Eligibility-related denials occur when insurance coverage is inactive, incorrect, or does not align with the date of service. In cardiology practices, these denials often result from incomplete front-end verification and quickly add avoidable volume to AR if not corrected early.
Prior Authorization and Referral Denials
Many cardiology diagnostic tests and procedures require prior authorization. When authorizations are missing, expired, or improperly linked to claims, payers deny services outright, delaying reimbursement and increasing follow-up workload.
Medical Necessity Denials
Medical necessity denials are common in cardiology, particularly for imaging, stress testing, and interventional procedures. These denials typically stem from documentation gaps or payer-specific coverage policies that require clear clinical justification.
Coding, Modifier, and Bundling Denials
Incorrect CPT selection, modifier misuse, or unbundled services frequently trigger cardiology claim denials. Given the complexity of cardiac procedures, even minor coding errors can lead to rejections or reduced payments.
Duplicate and Technical Claim Denials
Duplicate billing, formatting errors, or missing claim information can cause technical denials. While these denials are often preventable, they still slow down the revenue cycle and contribute to AR aging when not addressed promptly.
Shifting from Reactive Appeals to Root-Cause Analysis
Effective denial management focuses on identifying patterns rather than repeatedly fixing the same errors. By analyzing denials by payer, procedure, and provider, cardiology practices can correct workflow issues upstream and reduce future AR risk.
AR Management Trends Shaping Cardiology Practices in 2026
Automation and Predictive Analytics
In 2026, automation is no longer a luxury for cardiology practices it is a necessity for protecting accounts receivable. As claim volumes grow and payer rules become more complex, cardiology billing teams are increasingly relying on automated tools to support AR management for cardiology practices. Predictive analytics plays a key role by flagging claims that are likely to be denied based on payer behavior, coding patterns, or missing documentation. This allows billing teams to correct issues before submission rather than chasing denials weeks later. When used correctly, automation helps reduce rework, shortens payment cycles, and strengthens overall cardiology AR management without replacing the expertise of experienced billers.
Centralized and Outsourced AR Support
Staffing shortages and high turnover continue to strain in-house billing teams, making centralized and outsourced AR management for cardiology a growing trend in 2026. Many cardiology practices are shifting toward dedicated AR teams that focus exclusively on follow-up, appeals, and payer communication. Centralized AR workflows ensure consistent follow-up across all aging buckets and payer types, reducing the risk of claims slipping through the cracks. Outsourced AR management for cardiology also provides access to specialized knowledge of cardiology billing rules and payer-specific requirements, helping practices reduce AR aging while maintaining compliance.
Data-Driven Performance Monitoring
Data visibility has become essential for effective cardiology revenue cycle management. Advanced AR dashboards now allow practices to track key metrics such as days in AR, denial rates, payer turnaround times, and underpayments in real time. Instead of relying on reactive reports, leadership teams can use data-driven insights to identify bottlenecks, adjust staffing, and address payer performance issues proactively. For cardiology practices, consistent performance monitoring turns AR management from a reactive task into a strategic function that supports predictable cash flow and long-term financial stability.
State-Level Insights into Cardiology AR Performance
Understanding the regional payer behavior allows practices to tailor cardiology AR management strategies to local conditions and improve outcomes.
State-Level Insights into Cardiology AR Performance
| State | Cardiology AR Challenges | Payer Mix & Trends | AR Management Focus Areas |
| California | High denial rates due to complex managed care contracts, strict authorization requirements, and frequent medical necessity reviews for cardiac diagnostics and imaging. | Heavy presence of commercial HMOs, Medicare Advantage plans, and Medicaid managed care (Medi-Cal). | Strong pre-authorization workflows, payer-specific denial tracking, and tighter documentation alignment for cardiology procedures. |
| Texas | High claim volume and delayed reimbursements caused by fragmented payer rules and increasing Medicare Advantage penetration. | Large mix of Medicare, Medicare Advantage, and commercial PPO plans. | Proactive AR follow-up for cardiology claims, denial trend analysis by payer, and faster escalation for underpaid claims. |
| Florida | Elevated Medicare and Medicare Advantage denials related to medical necessity and bundled cardiology services. | High Medicare and Medicare Advantage enrollment due to aging population. | Focus on Medicare cardiology AR challenges, clean claim submission, and timely appeal management to reduce AR aging. |
| New York | Slower AR turnaround due to complex commercial payer policies and strict state-specific compliance requirements. | Strong commercial payer presence with Medicaid managed care programs. | Centralized AR workflows, improved coordination between coding and AR teams, and detailed payer follow-up documentation. |
| Pennsylvania | Increasing administrative burden from value-based reimbursement models impacting AR reconciliation timelines. | Balanced mix of commercial payers, Medicare, and emerging value-based contracts. | Enhanced reporting for cardiology revenue cycle management, reconciliation of quality-based payments, and consistent AR monitoring. |
| Illinois | Higher denial volumes linked to authorization and eligibility gaps for cardiology diagnostics. | Mix of commercial insurers and Medicare Advantage plans. | Front-end eligibility verification, authorization tracking, and denial prevention strategies in cardiology AR management. |
| Arizona | Growing AR backlogs due to rapid Medicare Advantage growth and evolving payer rules. | Increasing Medicare Advantage and Medicare patient population. | Focused AR follow-up for cardiology, payer education, and tighter medical necessity documentation. |
Preparing for the Future of Cardiology AR Management
As value-based care models expand, cardiology revenue cycle management will require tighter alignment between documentation, quality reporting, and reimbursement. Practices that invest in strong AR management for cardiology practices today will be better positioned to adapt to future changes.
How Cloud RCM Solutions Supports Cardiology AR Management
Cloud RCM Solutions partners with cardiology practices to strengthen AR management for cardiology practices through a strategic, specialty-focused approach. Rather than offering a generic solution, Cloud RCM evaluates each practice’s payer mix, procedure volume, and existing workflows to identify targeted improvements.
Specialty-Focused Cardiology AR Expertise
Cloud RCM cardiology billing support is designed to address the unique challenges of cardiovascular care. From bundled procedures to payer-specific policies, Cloud RCM understands the nuances of cardiology billing and AR services.
Proactive AR Follow-Up and Denial Prevention
Cardiology AR services by Cloud RCM focus on prioritizing high-value claims, analyzing denial trends, and improving follow-up efficiency. This approach helps practices reduce AR days in cardiology practices without overwhelming internal staff.
Transparent Reporting and Scalable Support
Cloud RCM Solutions provides clear reporting and performance tracking, allowing practices to monitor progress and adjust strategies as needed. As outsourced cardiology AR experts, Cloud RCM supports sustainable revenue cycle improvements rather than short-term fixes.
Final Thoughts:
AR management for cardiology practices in 2026 is no longer just an administrative task; it’s a strategic driver of revenue and financial stability. Rising denials, complex payer rules, and growing patient responsibility demand proactive workflows, denial prevention, and data-driven follow-up. Practices that address these challenges head-on reduce AR aging, improve cash flow, and maintain the operational resilience needed to focus on delivering exceptional cardiac care.
Don’t let denials and delayed payments hold your practice back. Partner with Cloud RCM Solutions to streamline cardiology AR, recover revenue faster, and gain complete visibility into your accounts receivable.
FAQ’s
Why is AR management more challenging for cardiology practices?
Cardiology billing involves complex procedures, multiple CPT codes, modifiers, and bundled services. Coupled with payer-specific rules, Medicare Advantage requirements, and high-denial risk, this complexity makes AR management particularly challenging for cardiovascular clinics.
How do patient responsibilities impact cardiology AR?
With high-deductible health plans, patients are responsible for a larger portion of cardiac care costs. Uncollected patient balances contribute to AR aging. Clear upfront communication, eligibility verification, and timely patient billing are critical for reducing patient AR.
What role does technology play in cardiology AR management?
Automation and predictive analytics allow billing teams to flag claims likely to be denied, streamline follow-up workflows, and reduce human error. Data-driven dashboards give leadership visibility into AR performance, denial trends, and payer turnaround times.
Should cardiology practices outsource AR management?
Outsourcing AR management is a growing trend, especially for practices facing staffing shortages. Specialized AR teams bring expertise in cardiology billing, payer-specific rules, denial prevention, and centralized follow-up, helping practices reduce AR aging and improve cash flow.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine