If you’re an Allergy & Immunology specialist seeking to boost revenue and reduce billing stress, CloudRCM is your trusted partner. We deliver specialized allergy & immunology medical billing and full RCM services designed for your unique coding, compliance, and payer challenges. In this blog, we’ll explain why allergy and immunology billing is different, share recent data, and reveal strategies to improve collections and cash flow.
Why Allergy and Immunology Billing Is Different
Allergy and Immunology practices manage a unique mix of services that require precise billing and coding. On the allergy side, this can include diagnostic testing, skin prick panels, patch testing, immunotherapy builds, and allergen extract preparation.
On the immunology side, services often extend to diagnosing and treating immune deficiencies, autoimmune diseases, and complex immunologic conditions, which may involve advanced lab testing, prolonged patient management, and biologic or immune-modulating therapies.
Each of these services comes with distinct CPT coding rules, documentation requirements, and payer-specific coverage criteria.
For example:
- Allergy injections (CPT 95115, 95117) are frequently denied when billed alongside an office visit on the same day unless the visit represents a separately identifiable service.
- Immunology services, such as comprehensive immune function panels, immunoglobulin infusions (CPT 96365, 96366), or specialty biologic administration, often require prior authorization and must meet strict medical necessity guidelines to qualify for coverage.
Common CPT Codes in Allergy & Immunology Billing
Accurate CPT coding is essential for getting reimbursed quickly in allergy & immunology practices. Below is a quick reference table of frequently used codes, along with billing tips to reduce denials:
| Service | CPT Code | Billing Tip |
| Allergy Skin Prick Test | 95004 | Document allergens tested, method (prick/puncture), and number of tests performed. Bill per allergen. |
| Allergy Intradermal Test | 95024 | Specify allergen and number of tests. Bill per allergen tested, not per injection site. |
| Allergen Immunotherapy – Single Injection | 95115 | Use only for one injection. If multiple, use 95117 in combination. Append modifier if billed with an E/M visit on the same day. |
| Allergen Immunotherapy – Multiple Injections | 95117 | Use when two or more injections are given during the same encounter. Cannot be billed with 95115 on the same day. |
| Allergen Extract Preparation (Single Dose) | 95165 | Bill per dose/vial prepared. Track the exact number to avoid overbilling and stay within payer limits. |
| Allergen Extract Preparation (Multiple Doses) | 95166 | Use for the preparation of multiple doses for the same patient during the same session. Follow payer rules for dose limits. |
| Immunoglobulin Infusion – Initial Hour | 96365 | Requires detailed documentation of infusion start/stop times and drug lot numbers. Often requires prior authorization. |
| Immunoglobulin Infusion – Additional Hour | 96366 | Bill for each additional hour after the initial infusion. Maintain clear infusion logs. |
| Patch Testing | 95044 | Document allergens applied and the total number of tests. Bill per allergen. |
| Drug Challenge Test | 95076 | Requires documentation of dosing increments and patient monitoring. May require pre-authorization for certain drugs. |
Common Challenges in Allergy and Immunology Billing
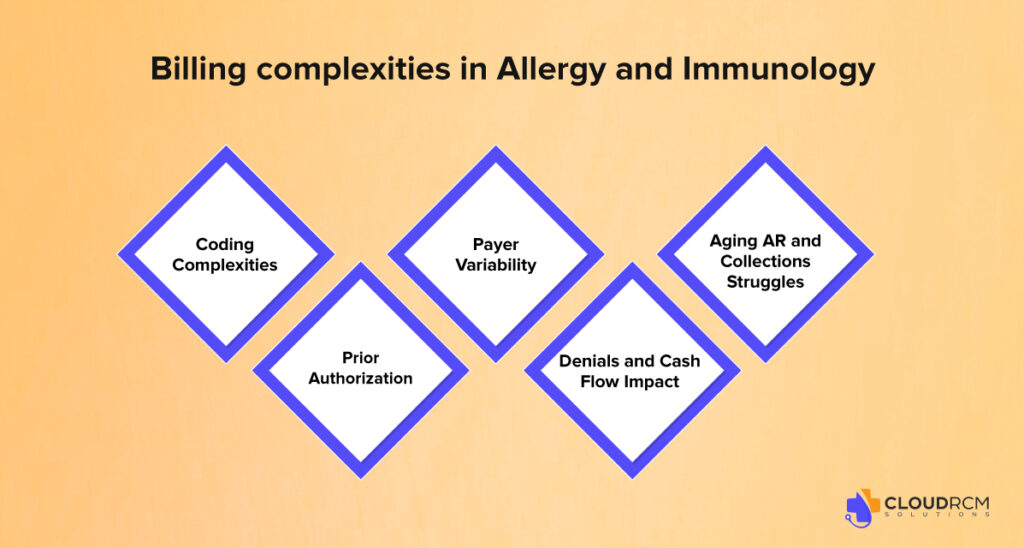
Billing for Allergy & Immunology services is far from straightforward. Providers often encounter multiple hurdles that can slow down payments, increase denials, and drain valuable administrative resources. Understanding these challenges is the first step toward improving your revenue cycle management and reducing billing stress.
Coding Complexities: (Same-Day Visits, Biologics & Telehealth)
Billing for allergy injections alongside office visits often results in denials unless properly documented with modifiers. Biologics and immune therapies require accurate CPT codes and payer-specific compliance. Telehealth billing is also tricky due to varying payer rules on eligible services and modifiers, leading to frequent claim rejections.
Prior Authorization
Many high-cost treatments, such as biologics and immunoglobulin infusions, require prior authorization. A 2023 MGMA study found that up to 60% of denials in specialty practices stem from missing or incomplete prior authorizations, causing delays and lost revenue.
Payer Variability: (Serum Prep and Dosing Limits)
Insurers differ widely in their approaches to serum preparation billing, vial caps, and bundling rules. Without a clear understanding of each payer’s policies, practices, and risk, claims are frequently denied.
Denials and Cash Flow Impact
Specialty practices face denial rates of 12-15%, nearly double the primary care average. Denials lead to costly resubmissions and delayed payments, putting pressure on cash flow and practice operations.
Aging AR and Collections Struggles
Claims unpaid after 60-90 days are harder to collect. Many allergy and immunology providers lack automated follow-ups or dedicated teams to manage aging AR, resulting in lost revenue and operational challenges.
Compliance Risks in Allergy & Immunology Billing
Allergy and immunology billing isn’t just about getting paid; it’s about staying compliant with payer and regulatory guidelines. Even small errors can trigger audits, recoupments, or penalties. Common compliance pitfalls include:
- Overbilling for Serum Preparation: Billing for more vials than prepared or exceeding payer dosing limits.
- Allergy Shots + E/M Visits: Failing to append the correct modifier when billing both on the same day, leading to improper payment or audit flags.
- Biologics Without Prior Authorization: Administering high-cost treatments before payer approval can result in full claim denials and unrecoverable costs.
- Incomplete Documentation: Missing elements like lot numbers, dosing schedules, or medical necessity notes.
Why Specialized Billing Matters for Allergy & Immunology Practices
The landscape of allergy and immunology billing is evolving fast. Recent data shows that without specialized, technology-driven billing solutions, many practices risk falling behind, losing revenue, and facing operational strain. Here’s why:
Rising Costs and Increased Administrative Burden
A 2024–2025 Medical Group Management Association (MGMA) survey reveals that medical practice operating costs have risen by nearly 8% annually, with billing and administrative expenses driving much of this growth. Allergy & immunology practices, with their complex coding and prior authorization requirements, are especially affected.
Growing Trend of Outsourcing and Automation
To combat these challenges, over 65% of specialty practices now outsource at least part of their billing process or use automated tools, a sharp increase from previous years. This shift is a clear sign that manual billing workflows are no longer sustainable.
AI and Automation: Reducing Denials, Speeding Payments
Advanced AI-powered billing platforms are helping practices reduce claim denials by identifying coding errors before submission. According to industry reports, automation can cut denial rates by up to 30% and accelerate payment cycles by 20–25%. For allergy & immunology providers, this means fewer rejected claims for complex immunotherapy or biologic treatments and faster cash flow.
Telehealth Billing Trends and Payer Policy Changes
Telehealth has become a vital part of allergy and immunology care, especially for follow-ups and patient education. However, evolving payer policies continue to complicate billing. Practices must stay updated on telehealth coverage, eligible CPT codes, and required modifiers to avoid costly denials.
Proven Tips to Improve Allergy and Immunology Billing Solutions
Billing for allergy and immunology can be very tricky, but with the right approach, you can make the process smoother and keep a good revenue flow for your practice. Here are some effective steps to help you optimize allergy & immunology billing and get paid faster:
Review Claims Before Sending Them
Taking a little extra time to double-check claims and coding can save you from costly mistakes down the line. Regular reviews help catch errors early, so your claims stand a better chance of getting approved the first time.
Use Specialty-Specific Documentation Templates
Having clear, easy-to-follow templates for documenting patient visits ensures nothing important gets missed. This helps your coding stay accurate and keeps payers happy.
Get Prior Authorizations Early
Waiting until the last minute for prior approvals can slow things down. By tying prior authorization to the scheduling process, you reduce delays and make sure treatments like biologics and infusions get approved before the appointment.
Stay on Top of Denials and Appeals
Denials happen, but a good system for tracking them and appealing when appropriate can recover lost revenue. Focus especially on common issues like allergy injections or lab tests.
Consider Outsourcing Your Billing and Collections
Partnering with a specialized billing service can take a huge weight off your shoulders. Outsourcing helps ensure claims are submitted accurately and followed up quickly, reducing errors and speeding up payments. It frees your team from administrative burdens so you can focus more on patient care.
How CloudRCM Supports Allergy & Immunology Practices
CloudRCM knows that allergy and immunology billing is unique. Our experts specialize in this area, handling the complex coding and payer rules so you don’t have to.
We create tailored RCM processes designed for your specific services and insurance requirements, helping improve claim accuracy and speed payments.
From prior authorizations to denials and collections, our technology-driven approach reduces admin work and keeps your practice’s revenue healthy. Outsource your allergy billing company to CloudRCM and focus more on patients while we manage your billing challenges.
Final Thought:
Mastering allergy and immunology billing takes more than just submitting claims; it requires precision, compliance, and a strategy tailored to your specialty. By partnering with experts who understand your unique challenges, you can improve operations, reduce stress, and boost collections.
Take the Next Step
CloudRCM delivers specialized allergy & immunology billing solutions designed to help your practice thrive. Let us handle the complexities so you can focus on delivering exceptional patient care.
Schedule an appointment today to see how we can optimize your revenue cycle.
FAQs
What is the most common billing mistake in allergy practices?
Incorrect modifier usage when billing allergy injections with office visits.
Do insurance plans cover allergy testing?
Most do, but coverage varies by payer, plan type, and documented medical necessity.
How can I reduce denials for allergy injections?
Ensure proper coding, use required modifiers, and follow payer-specific rules.
Should I outsource my allergy billing or keep it in-house?
Outsourcing often reduces errors, speeds payments, and eases administrative workload.
Which CPT codes are used most in allergy & immunology billing?
Common codes include 95004, 95115, 95117, 95165, 96365, and 96366.
How long does it take to get paid for allergy services?
With clean claims, payments typically arrive within 14–30 days, depending on the payer.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine