Applied Behavior Analysis (ABA) therapy has become a critical service for individuals with autism spectrum disorder (ASD) and related developmental conditions. As demand for ABA services continues to rise across the U.S., providers face a different kind of challenge behind the scenes: billing and coding complexity.
ABA therapy billing is not like general outpatient billing. It involves time-based CPT codes, strict authorization rules, credentialing requirements, state-specific Medicaid policies, and frequent payer audits. Even small errors can lead to denied claims, delayed payments, or lost revenue.
For ABA practices already stretched by staffing shortages, administrative burdens, and payer pressure, billing issues can quietly drain cash flow. That’s why accurate, specialty-focused ABA therapy billing and coding services are no longer optional; they’re essential.
Why ABA Therapy Billing Is Especially Complex
ABA therapy billing is built on rules that differ significantly from many other behavioral health services. Payers scrutinize ABA claims closely due to high utilization, long treatment durations, and variable provider models.
Key challenges in ABA billing include:
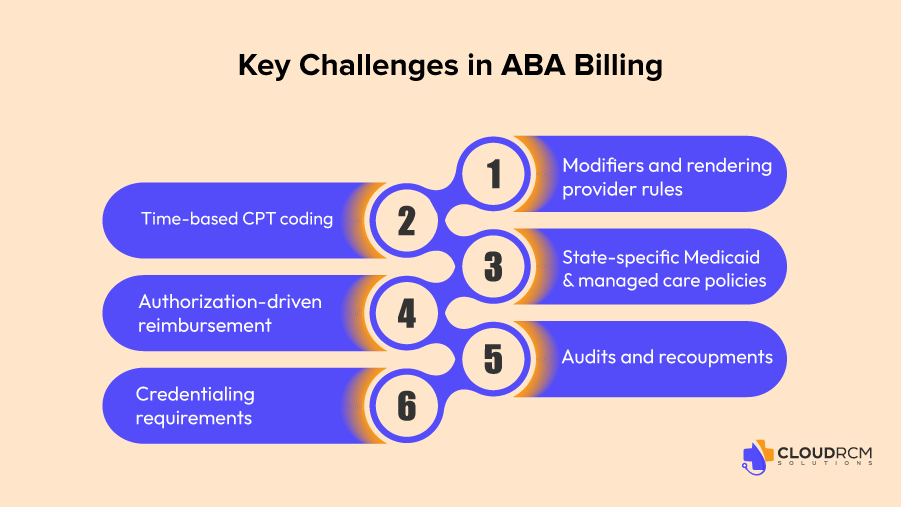
- Time-based CPT coding with strict unit calculations
- Authorization-driven reimbursement, often tied to treatment plans
- Credentialing requirements for BCBAs, BCaBAs, and RBTs
- Modifiers and rendering provider rules
- State-specific Medicaid and managed care policies
- Frequent audits and recoupments
According to industry data, behavioral health services, including ABA, experience denial rates ranging from 15% to 25% on first submission, largely due to authorization, documentation, and coding errors. Claims that age beyond 90 days have less than a 20% chance of full recovery, making timely and accurate billing critical.
Understanding ABA Therapy CPT Codes and Billing Structure
ABA services are billed primarily using CPT codes in the 97151–97158 range, along with adaptive behavior treatment and assessment codes. These codes are time-based and role-specific, which means billing accuracy depends heavily on documentation and supervision requirements.
Common ABA Therapy CPT Cheat Codes
| CPT Code | Description |
| 97151 | Behavior identification assessment |
| 97152 | Adaptive behavior treatment by protocol (RBT-delivered) |
| 97153 | Adaptive behavior treatment with protocol modification |
| 97154 | Group adaptive behavior treatment |
| 97155 | Adaptive behavior treatment with protocol modification by BCBA |
| 97156 | Family adaptive behavior guidance |
| 97157 | Multiple-family group adaptive behavior treatment |
| 97158 | Group adaptive behavior treatment with protocol modification |
Each code has specific rules regarding:
- Who can render the service
- Who must supervise
- How time is calculated
- Whether modifiers are required
- Whether services must align with the authorized treatment plan
Incorrect code selection, unit miscalculations, or missing supervision documentation are among the top reasons ABA claims are denied.
Authorization Management: A Major Revenue Risk for ABA Practices
Most ABA therapy services require prior authorization, often tied to:
- Initial assessments
- Treatment plan approvals
- Recertifications (typically every 6 months)
- Session limits by code and provider type
Missed or expired authorizations are one of the biggest causes of non-payment in ABA billing.
Common authorization issues include:
- Services rendered outside approved dates
- Units exceeding authorized limits
- Mismatch between authorized codes and billed codes
- Lack of updated treatment plans
Because ABA therapy is ongoing and long-term, authorization tracking must be proactive. Once a service is delivered without valid authorization, recovery is often impossible, especially with Medicaid and managed care plans.
State-Specific ABA Billing Challenges
ABA therapy coverage and billing rules vary widely by state. Medicaid expansion, managed care penetration, and autism mandate laws all impact reimbursement.
States with Higher ABA Billing Complexity
- California: Strict Medicaid (Medi-Cal) documentation rules, frequent audits, and managed care carve-outs
- Texas: Complex Medicaid MCO structure and authorization variability
- Florida: High Medicaid enrollment and payer-specific ABA policies
- New York: Heavy documentation requirements and oversight
- Illinois: Expanding managed care with evolving ABA coverage rules
ABA practices operating across multiple states often struggle to keep up with payer-specific and state-specific changes, increasing denial risk when billing is handled generically.
Credentialing and Rendering Provider Errors
ABA therapy relies on a team-based care model, but billing rules still require clarity around who rendered the service and who supervised it.
Common credentialing-related billing errors include:
- Billing under the wrong NPI
- Using uncredentialed RBTs
- Missing BCBA supervision documentation
- Incorrect modifier usage
Payers are increasingly strict about rendering provider accuracy, especially for Medicaid and Medicare Advantage plans. Credentialing gaps often lead to denials that cannot be appealed successfully.
Documentation: The Foundation of Clean ABA Claims
ABA billing lives and dies by documentation. Payers expect session notes to clearly support:
- Medical necessity
- Time spent
- Services rendered
- Alignment with the treatment plan
- Supervision and protocol modification (when applicable)
Weak or inconsistent documentation leads to:
- Denials
- Post-payment audits
- Recoupments months after payment
For ABA providers, billing teams must understand clinical workflows well enough to flag documentation gaps before claims are submitted.
How ABA Billing Issues Impact Cash Flow
When ABA billing breaks down, the financial impact can be severe:
- Delayed reimbursements increase A/R days
- Denials pile up and overwhelm staff
- Underpayments go unnoticed
- Revenue becomes unpredictable
Industry benchmarks show that 3–5% of annual revenue is lost to underpayments alone, often because practices lack the time or systems to audit payments against contracted rates.
For ABA practices operating on tight margins, these losses limit growth, staffing, and patient access.
Why Generic Billing Services Fall Short for ABA Therapy
Many ABA practices start with general medical billing services, only to realize later that their unique needs aren’t being met.
Generic billing teams often struggle with:
- Time-based unit calculations
- ABA-specific CPT rules
- Authorization tracking
- State Medicaid differences
- Audit preparedness
ABA billing requires specialty knowledge. Without it, practices pay the price through denials, aging A/R, and lost revenue.
How Cloud RCM Solutions Supports ABA Therapy Providers
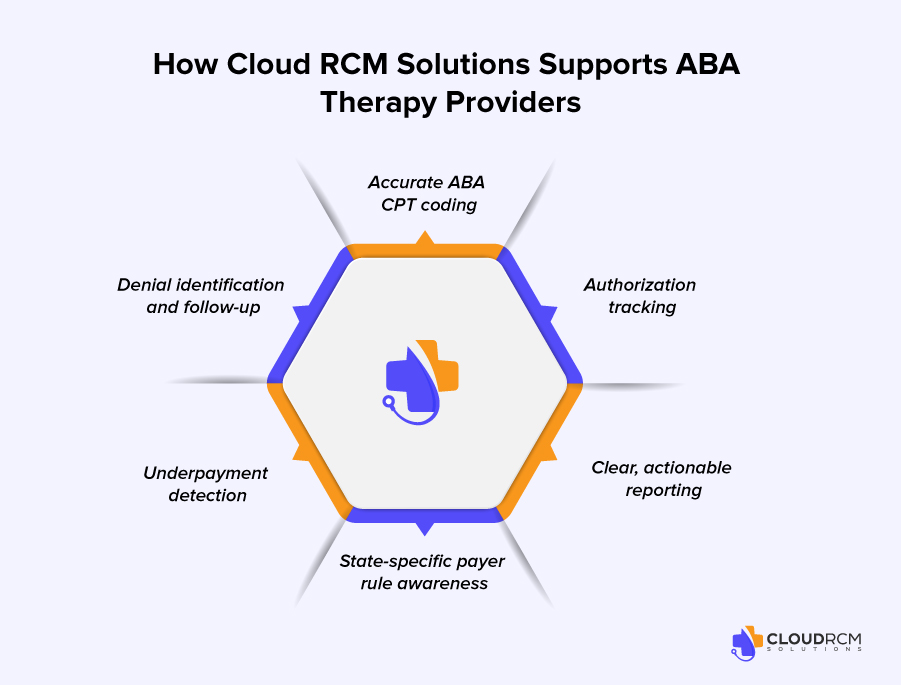
Cloud RCM Solutions provides specialty-focused ABA therapy billing and coding services designed to reduce revenue leakage while supporting long-term financial stability.
Rather than applying a one-size-fits-all billing approach, Cloud RCM Solutions focuses on:
- Accurate ABA CPT coding and unit calculations
- Authorization tracking and compliance support
- Denial identification and follow-up
- Underpayment detection
- State-specific payer rule awareness
- Clear, actionable reporting
Cloud RCM Solutions works alongside existing teams, integrating into current workflows instead of disrupting them. The goal is not shortcuts, but consistency, accuracy, and visibility.
ABA Billing, Technology, and Smarter Workflows
Modern ABA billing requires more than manual follow-ups. Cloud RCM Solutions leverages intelligent automation to:
- Track claim status in real time
- Flag aging claims early
- Prioritize high-risk and high-value accounts
- Surface denial trends by payer and state
This approach allows billing staff to focus on complex issues while technology handles repetitive tracking and alerts.
What ABA Practices Gain from Better Billing Visibility
When ABA billing is managed correctly, practices benefit from:
- Faster reimbursements
- Fewer denials
- Lower A/R days
- Improved cash flow
- Stronger audit readiness
Even modest improvements, such as reducing denials by 5% or recovering underpayments, can translate into significant annual revenue gains for mid-sized ABA organizations.
The Bigger Picture: Billing as a Growth Strategy
ABA therapy demand continues to rise nationwide. Practices that want to scale sustainably must treat billing as a financial strategy, not an afterthought.
Clean claims, proactive authorization management, and accurate coding create the foundation for:
- Expanding services
- Hiring additional clinicians
- Entering new states
- Serving more patients
Without stable revenue, growth becomes risky.
Final Thoughts: ABA Billing Requires Focus and Expertise
ABA therapy billing and coding is complex, highly regulated, and constantly evolving. Practices that rely on generic billing processes often experience preventable revenue loss.
Specialty-focused billing, combined with smarter workflows and clear reporting, helps ABA providers protect margins while staying compliant.
Cloud RCM Solutions supports ABA practices by strengthening billing operations, improving visibility, and reducing financial friction so providers can stay focused on delivering quality care.
FAQ’s
What is ABA therapy billing and coding?
ABA therapy billing and coding involves submitting claims for Applied Behavior Analysis services using the correct CPT codes, modifiers, authorizations, and payer rules to ensure accurate reimbursement.
Why is ABA therapy billing so complex?
ABA billing is complex due to strict authorization requirements, time-based codes, frequent payer policy changes, and state-specific Medicaid rules.
Which CPT codes are commonly used in ABA therapy billing?
Common ABA therapy CPT codes include 97151, 97153, 97155, 97156, and 97158, depending on the service provided and supervision level.
How do authorizations impact ABA therapy reimbursement?
Missing or expired authorizations are one of the leading causes of ABA claim denials, making authorization tracking critical for revenue protection.
How does Medicaid affect ABA therapy billing?
Medicaid ABA billing varies by state and often includes strict documentation, supervision, and credentialing requirements that must be followed precisely.
Why are ABA therapy claims frequently denied?
Denials often occur due to authorization issues, documentation gaps, incorrect CPT usage, or payer-specific billing rules.
Can underpayments occur in ABA therapy billing?
Yes, underpayments are common and often go unnoticed without proper contract and payment review.
How does Cloud RCM Solutions support ABA therapy practices?
Cloud RCM Solutions helps ABA practices improve claim accuracy, manage authorizations, reduce denials, and gain better visibility into A/R performance.
Is outsourcing ABA therapy billing cost-effective?
Outsourcing can reduce administrative burden, improve collections, and allow providers to focus more on patient care rather than billing issues.

 Medical Billing
Medical Billing Medical Coding
Medical Coding Medical Audit
Medical Audit Provider Credentialing
Provider Credentialing Denial Management
Denial Management A/R Follow-up
A/R Follow-up Private Practice
Private Practice Patient Help Desk
Patient Help Desk Customized Reporting
Customized Reporting Out-of-Network Billing
Out-of-Network Billing Internal Medicine
Internal Medicine Pediatrics
Pediatrics Radiology
Radiology Surgery
Surgery Emergency Medicine
Emergency Medicine Anesthesiology
Anesthesiology Cardiology
Cardiology Orthopedic
Orthopedic Psychiatry
Psychiatry Dentistry
Dentistry OB-GYN
OB-GYN Family Medicine
Family Medicine