Are medical billing errors holding you back from maximizing your Revenue Cycle Management (RCM) potential? Hold on! We are just here to unveil the strategies that can help you steer clear of medical billing errors.
Join us on this enlightening journey as we first mentioned the possible medical billing errors in RCM and unlock the secrets to error-free RCM. We also empower healthcare providers to optimize financial performance. Get ready to discover the key practices that can safeguard your revenue and lift up your practice to new heights of success in the complex realm of medical billing.

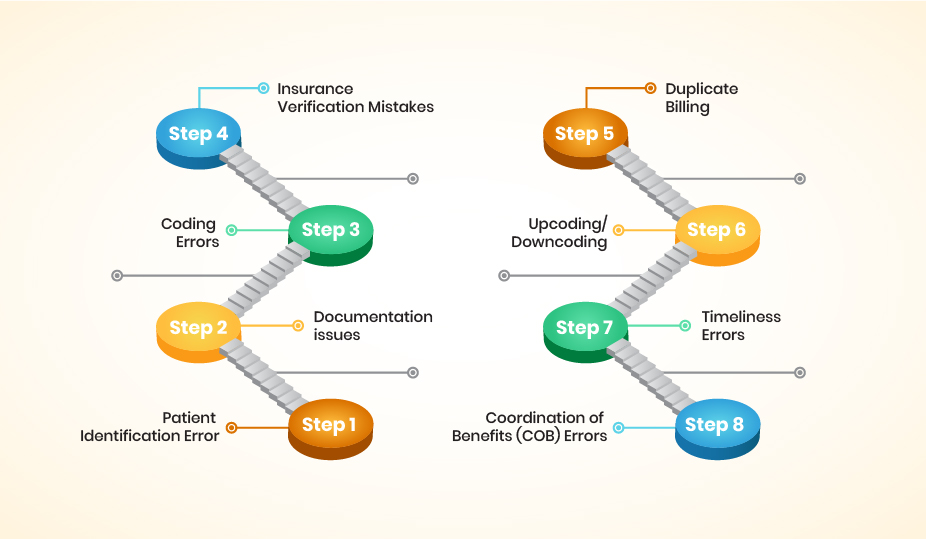
Patient identification errors in RCM occur due to inaccuracies or mistakes in identifying your correct information and linking them to your medical records. It may include your misspelled name, incorrect date of birth, or incomplete information.
False patient identities can result in claim denials, incorrect billing, or privacy breaches. It can also lead to delays in processing claims and miscommunication between you and healthcare providers.
Insufficient or incomplete information that fails to support billed services or lacks your necessary details. These documentation issues can lead to claim denials, delayed payments, or potential compliance issues.
Without sufficient and accurate documentation, healthcare providers may struggle to support the services billed. It could result in decreased reimbursement or non-payment for services rendered. Furthermore, the documentation’s missing or incomplete details may hinder proper coding and billing, causing delays and potential revenue loss.
As you face, coding errors are the inaccuracies or mistakes in assigning diagnostic and procedural codes to medical services provided. These errors can occur due to incorrect code selection, inadequate documentation, and limited knowledge of coding guidelines.
Incorrect coding can result in claim denials, undercoding (leading to revenue loss), or overcoding (which may result in potential legal and compliance issues). Additionally, coding errors can also impact your data accuracy, quality reporting, and overall healthcare analytics.
The errors or inaccuracies occur in verifying your insurance coverage and entering the insurance information into the billing system. These insurance verification mistakes can include incorrect entry of insurance details, failure to verify eligibility, or overlooking changes in insurance coverage.
If insurance information is entered incorrectly or not verified, it can result in claim rejections, payment delays, or coverage denial. Additionally, overlooking changes in insurance coverage can lead to incorrect billing, causing financial strain on the healthcare provider and the patient.
Duplicate billing errors in RCM occur when multiple claims are submitted for the same medical service or procedure. This happens due to system glitches, human error, or failure to identify duplicate entries in the billing process.
Submitting multiple claims for the same service can result in overpayment, reimbursement delays, or even potential legal and compliance issues. It can also confuse insurance companies, leading to claim denials or audits.
Upcoding and downcoding errors occur when service codes are inaccurately assigned, failing to reflect the level of care or services provided. Upcoding involves using a higher-level code, while downcoding entails using a lower-level code than necessary.
Upcoding can lead to overbilling, potential fraud, and increased scrutiny from payers or auditors. Downcoding, on the other hand, may result in underbilling and potential revenue loss.
Timeliness errors in RCM occur when medical billing claims are not submitted within the required timeframes. Late claim submission can result in missed opportunities for timely reimbursement.
In addition, Timeliness errors can disrupt cash flow, impact revenue cycle performance, and hinder the financial stability of healthcare providers.
Coordination of Benefits (COB) errors in RCM occur when there are inaccuracies or mistakes in identifying primary and secondary insurance coverage for you. These errors can result in your claim processing delays, denials, or incorrect reimbursement.
Failure to accurately determine primary and secondary insurance coverage can lead to confusion and complications in the billing process. COB errors may result in claims being sent to the wrong insurance carrier, leading to claim rejections or delays in payment.
As you’re facing medical billing errors in RCM, these strategies will help you overcome all the medical billing and maximize your Revenue Cycle Management (RCM) potential.

Accurate patient identification, such as correct names, dates of birth, and other relevant information, prevents medical billing errors in RCM. Through this, healthcare providers can minimize mistakes in billing processes and avoid claim denials or delays.
With accurate patient identification, RCM workflows become streamlined and reduce the risk of errors. By verifying patient identities accurately, healthcare providers can ensure that billing information aligns with the correct individual, mitigating confusion or mix-ups. This accuracy in patient identification enhances the overall financial performance of healthcare providers.
Accurate documentation includes patient encounters, diagnoses, treatments, medical history, and payment records. It enables healthcare providers to minimize errors and ensure proper coding and billing.
With robust documentation practices, healthcare providers can establish a strong foundation for accurate and compliant medical billing. This can lead to improved financial outcomes and streamlined RCM processes.
Ongoing staff training includes regular training sessions and educational opportunities. By this, healthcare providers can keep their staff updated with the latest coding guidelines, billing regulations, and best practices.
Continuous training helps you to stay knowledgeable and proficient in your roles, reducing the risk of coding errors and documentation deficiencies. It ensures you have the necessary skills and knowledge to navigate complex RCM processes accurately and efficiently.
Precise and appropriate code assignment for diagnoses and services minimizes claim denials, billing discrepancies, and compliance issues for healthcare providers. Moreover, You can reduce claim denials and medical billing discrepancies by appropriate code assignment for diagnoses and services.
Accurate coding ensures that services are properly documented and billed, reflecting the level of care and resources utilized. It helps avoid undercoding, which can result in revenue loss. On the other hand, overcoding may lead to audits or legal repercussions. With attention to coding accuracy, you can optimize reimbursement and streamline your revenue cycle management processes.
Healthcare providers can proactively detect coding errors, documentation deficiencies, and other billing mistakes through regular audits. By reviewing claims, documentation, and billing practices, organizations can address issues promptly and implement corrective measures to improve overall accuracy.
This proactive approach helps minimize claim denials, optimize reimbursement, and maintain compliance with billing regulations. Regular reviews allow healthcare providers to refine workflows and implement strategies to enhance revenue cycle management practices.
Establishing effective communication channels between you, healthcare providers, and insurance companies minimizes the likelihood of misunderstandings and errors. Open and transparent communication allows for accurate exchange of information, clarifications, and resolution of any billing-related issues.
By fostering clear communication channels, you can improve the accuracy and efficiency of your billing processes. This helps prevent errors such as incorrect billing information, coverage misunderstandings, or claims processing delays.
Advanced software and tools for medical billing errors can help you to streamline processes, enhance accuracy, and mitigate the risk of errors. Technology solutions automate critical aspects of the billing workflow, such as claim submission, coding validation, and eligibility verification.
Implementing technology solutions also improves efficiency by eliminating manual tasks, reducing paper-based processes, and bolstering data accuracy and security. These tools reduce the likelihood of human error and ensure consistent adherence to coding guidelines and billing regulations.
By adhering to relevant laws and guidelines, healthcare providers can minimize the risk of non-compliance, claim denials, penalties, and legal consequences. Staying current with regulatory requirements can prevent errors such as false identification, incorrect coding, or fraudulent medical billing.
By implementing effective compliance programs, healthcare providers can ensure ethical and compliant billing practices in RCM. This will also enhance your trust in health providers and mitigate financial problems.
External experts can conduct thorough assessments of your RCM processes, identify areas for improvement, and provide helpful recommendations. Their expertise can help ensure proper coding, accurate documentation, and reduce the risk of errors in medical billing.
Furthermore, partnering with external experts can provide you with valuable insights and guidance to optimize your RCM practices. They can also help in minimizing errors, and streamlining RCM operations.
The key performance metrics and data related to the RCM, healthcare organizations can identify areas for improvement. In addition, it addresses bottlenecks and optimizes your medical billing processes.
A thorough analysis of revenue cycle performance helps identify trends, patterns, and potential issues that may lead to billing errors or inefficiencies. It enables healthcare providers to monitor claim denial rates, average reimbursement time, and billing accuracy.
Avoiding medical billing in RCM has equal importance as you depend on the billing and claim process, reimbursement accuracy, and streamlined workflows. By avoiding medical billing errors, you can increase revenue, optimize medical billing operations, and hit high efficiency in RCM.
When you are looking to find out the solutions for the medical billing errors in RCM, CloudRCM is a leading solution provider in the healthcare industry. With our advanced expertise in revenue management cycle, CloudRCM’s provide valuable and helpful solutions regarding medical billing concerns. Today explore CloudRCM’s solutions and get rid of medical billing errors in RCM.
To avoid medical billing errors in RCM you should ensure accurate documentation, coding, and billing practices. By implementing staff training programs, conducting regular audits, utilizing technology solutions could also be helpful to overcome these errors.
Medical billing errors can lead to claim denials, delayed payments, financial losses, compliance issues, audits, and reputational damage. They can disrupt cash flow, impact revenue cycle performance, and strain the financial stability of healthcare providers.
Technology solutions automate processes, streamline workflows, enhance data accuracy and security, and offer analytics capabilities. By leveraging technology, healthcare providers can minimize human error, ensure compliance, and improve efficiency in medical billing.
Ongoing staff training keeps healthcare professionals updated with coding guidelines, billing regulations, and best practices. It helps reduce coding errors, documentation deficiencies, and other common billing mistakes. Training programs empower staff with the necessary skills to navigate complex RCM processes accurately and efficiently.

Revenue Cycle Management (RCM), the method for handling healthcare claims adjudication, is the revenue generator for