What does it mean to be credentialed in medical billing? It's an initial step that helps doctors get paid by insurance company for their medical services. Credentialing checks if doctors have the right education and licenses to ensure they can provide quality care.
This blog will explore credentialing in medical billing. We’ll explore why it’s so important and how it helps both doctors, healthcare providers, and patients.
Plus, simplify your provider credentialing process with our expert Provider Credentialing Services. Our comprehensive solutions ensure accurate credentialing, reduce administrative burdens, and improve revenue cycle management.
Credentialing in medical billing is like getting a special element. This element helps doctors get paid by insurance companies for their work. It checks if doctors have the right education, experience and licenses.
When doctors get this key, they can receive payment from health plans. It’s a process to make sure they meet medical standards. This process helps patients to trust their doctors more.

Credentialing in medical billing delivers trust and efficiency. It assures quality care for patients and streamlines financial transactions.
Credentialing in medical billing proves that doctors are qualified and experienced. It shows they met all the necessary training and education standards. Patients feel safe as their health is in good hands.
When doctors are credentialed, it builds trust with patients. They know the doctor has the right skills and experience to treat them. This trust makes patients more likely to follow medical advice and also more trusting of their healthcare providers.
Credentialing healthcare simplifies the medical billing process and helps to overcome medical coding errors. It ensures that doctors are approved to bill insurance. This verifies that healthcare costs are covered easier for patients.
Credentialing medical billing makes sure that doctors can provide care and receive payment. It’s an excellent opportunity for doctors to join the healthcare team.
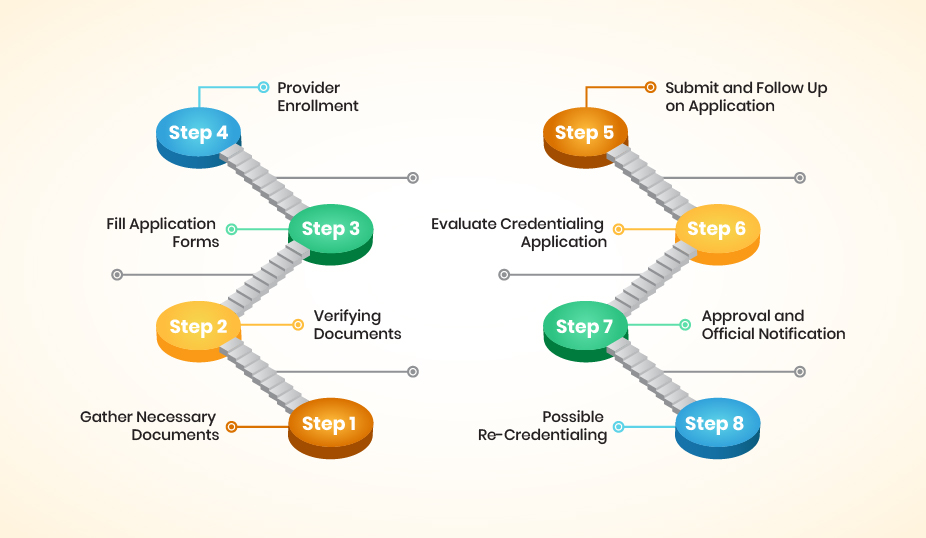
Every insurance company has its own requirements for the medical billing process. This could include licenses, certifications, and experience in medical billing. You should start by collecting information about the specific insurance companies you want to work with you.
Their websites or a call to the healthcare provider enrollment department can help you understand their requirements.
When you are well aware of what you need regarding provider credentialing services, you must collect all the documents that prove your qualifications and experience in medical billing services. This might include your medical billing CV, license, experience letter and certification, which would be proof for the insurance company.
Each insurance company will have its own application process. It might be online, on paper, or require a combination of both. You need to fill out the applications accurately and attach all the required documents.
Few insurance companies participate in CAQH. It’s a program that streamlines RCM credentialing and allows you to submit your information once. If it matches with the insurance eligibility verification, then know about the targeted insurance company and complete your profile.
After submitting your application, the insurance company will verify your information and credentials. This process can take several weeks or even months. Be patient, and keep track of your applications. You may need to follow up with the insurance company if you do not get a response in a reasonable amount of time.
Once you’re credentialed with an insurance company, you’ll need to keep your information and licenses up-to-date. As companies require periodic re-credentialing, You should make sure you know about their process and deadlines to avoid any interruptions in medical billing.
Once you’re credentialed with an insurance company, you’ll need to keep your information and licenses up-to-date. As companies require periodic re-credentialing, You should make sure you know about their process and deadlines to avoid any interruptions in medical billing.
Automated credentialing in medical billing streamlines the whole process. It uses automated credentialing software to manage tasks and reduces manual work.
Automated systems make credentialing faster and reduce waiting times. You won’t have to wait long to get things done. It allows healthcare providers to begin their services quicker. This efficiency helps get doctors and nurses to work faster and improve patient care.
AI helps avoid mistakes in paperwork by checking every detail with precision. With this system, you can check details carefully and accurately. This precision helps in maintaining high standards in medical billing services. Moreover, it builds trust among patients and insurance companies.
Advanced software for credentialing can save your valuable time. It makes the whole process more efficient. It also means you have less money for paper and mail and unnecessary expenses. These savings can be redirected towards better healthcare services or advanced medical equipment.

Automated credentialing in medical billing brings many benefits. It changes how healthcare providers handle their important paperwork.
Automated systems make the work pace fast, so tasks get done quicker. It helps reduce the payments delays. This means less waiting and more doing, which allows staff to allocate their time to patient care. Hospitals and clinics become more productive and serve more patients effectively.
Insurance eligibility verification software checks details very carefully and reduces mistakes to enhance the reliability of billing processes. This makes sure that each information is correct. Moreover, it builds confidence in medical billing accuracy among healthcare providers and insurers alike.
Everything can be seen in one place with automation. It is easy to manage credentials and keep records current. Tracking who is credentialed and who’s not becomes easier with simple compliance with regulations. This centralized approach reduces administrative burdens and improves operational efficiency.
When dealing with credentialing in medical billing, the healthcare provider must be well aware of the laws and rules. These make sure patients get safe and proper care. You need to stay updated on changes in laws. New rules can come out at any time. Provider credentialing services ensure that healthcare providers always meet the latest requirements.
First, you must follow privacy laws. These protect patient information from being shared incorrectly. Also, there are specific rules about healthcare providers. These rules help make sure doctors and nurses are qualified. Credentialing checks their education and experience to meet these standards.
The medical billing and coding process is a little bit complex and technical. Credentialing mistakes can lead to serious problems for healthcare providers.
This is a common and costly mistake. You must ensure you gather and submit all required documents mentioned in the application instructions. The missing documents can lead to delays and claim denials. You should always double-check everything before submitting your application.
Typos, errors in dates, or inconsistencies between documents can make you disqualified for the verification. You should always carefully review all information entered in applications and ensure it matches your licenses, certifications, and CV/resume exactly.
Your credentialing can take weeks or even months. You can’t miss the deadlines for submitting applications or responding to requests for additional information. Moreover, you should keep track of key dates and proactively follow up with insurance companies if necessary to avoid delays.
The provider credentials in medical billing regarding doctors and health services ready to bill insurance can be tricky. Let’s talk about why it’s tough and use simple terms so that everyone can understand it.
The provider credentialing in medical billing can be a slow and tedious process. Each insurance company has its own requirements and application procedures. This verification of your information can take weeks or even months. Moreover, it can be frustrating for new billers waiting to start working with specific insurance providers.
You should maintain accurate and up-to-date information across multiple applications. This includes licenses, certifications, experience details, and contact information. In this case, any discrepancies can lead to delays or rejections.
Insurance companies have varying provider credentialing requirements. It is difficult to keep track of what’s needed for each one. You might need to explore different websites, application forms, and contact information for each company.
The traditional manual credentialing process often lacks transparency. It can be difficult to track the status of your applications with different insurance companies. Moreover, it could cause delays or identify potential issues.
To achieve your claim successfully, your credentialing approach must be advanced and accurate according to the requirements. Here, we’ll explore strategies to prevent delays and keep your billing on track.
You need to learn about credentialing billing. It’s like making sure doctors and hospitals can get paid. Consider it a special pass to join the team. This pass allows them to work with insurance companies. For this, start this process early, as it can be time-consuming.
Next, it’s important to fill out every form with care and accuracy. If you make a mistake, it can cause payment delays or claim denials. You should always double-check your work before you send it. Moreover, you should provide all the needed documents without missing any.
For the claims, you should keep track of your application’s progress. You can call or email to check that things are going well for you. Call or email to check in if things seem slow. But it demands that you be persistent and patient.
The credentialing process in medical billing requires careful attention and smart strategies. Let’s dive into how the best practices of credentialing can smoother medical billing.
You should start early with your credentialing paperwork. Delays in the credentialing process can cause stress. If you have adopted best practices for provider credentialing, then these approaches will help you handle the paperwork challenges.
Next, your application process will be simple and clear. This approach saves time for everyone involved. A straightforward process leads to quicker approvals, benefiting your practice.
In the initial requirement for the healthcare provider to stay in touch with the credentialing team. If you have quick responses to patient questions, it helps to speed up the credentialing process. Regular check-ins show your commitment and can fix the credentialing errors.
Choosing CloudRCM for your medical billing credentialing services makes a big difference. They handle the tricky parts, so you don’t have to worry. With their help, your billing process becomes smoother and faster.
CloudRCM knows the ins and outs of credentialing in medical billing. They work hard to make sure your paperwork is right and submitted on time. This means you can focus more on patient care, and you are satisfied that the paperwork is in good hands.
The credentialing process in medical billing is currently a mandatory requirement for you. It makes sure doctors are ready and can get paid right away by insurance. This process keeps everyone satisfied, from doctors to patients.
CloudRCM stands out as the top choice for credentialing services in medical billing. Today, explore and join our services to see the difference for yourself.
Credentialing checks doctors’ skills and education before they start. It ensures they can provide safe, quality care. Patients feel more secure knowing their doctors are checked.
The credentialing process involves verifying doctors’ qualifications and backgrounds. It includes checking their education, training, and licenses. This process helps maintain high standards in healthcare.
Yes, credentialing is a crucial step in revenue cycle management (RCM). It ensures doctors are approved to bill insurance companies. Without it, billing and payment for services get complicated.
Medical billing handles charging and collecting money for healthcare services. Credentialing ensures doctors are qualified to provide these services. Both are vital for a smooth healthcare operation.
The credentialing process checks and approves healthcare providers’ qualifications. It’s key to ensuring patient safety and quality of care. This process is essential for healthcare trust and efficiency.
Credentialing proves you meet standards to bill insurance. It confirms your qualifications and trustworthiness. This step is crucial for your reimbursement and credibility.

Revenue Cycle Management (RCM), the method for handling healthcare claims adjudication, is the revenue generator for